I’ve noticed you’re probably wondering how Turkish clinics manage ten-plus hair transplants daily without sacrificing quality. It sounds impossible on the surface. But here’s what’s actually happening: they’re not cutting corners—they’re reimagining the entire surgical workflow. The answer lies in specialized staffing, parallel operations, and ruthless scheduling efficiency. Let me show you how.
The Turkish Hair Transplant Market Runs on Scale Economics
Because Turkey performs roughly 600,000 hair transplants annually—more than any other country in the world—clinics there operate on an entirely different economic model than those in North America or Europe.
High volume creates lower per-procedure costs. When a clinic performs dozens of transplants weekly, overhead spreads across many patients. Staff become specialized and efficient. Surgical teams develop rhythm and speed without sacrificing quality.
Economic incentives drive this scale. Turkish clinics compete on price while maintaining profitability through volume. This isn’t inherently bad—it explains why costs run 40–60% lower than Western clinics.
However, regulatory oversight matters here. Turkey’s Ministry of Health licenses clinics and enforces standards, but enforcement varies. Volume alone doesn’t guarantee quality. Understanding *why* clinics operate this way helps you evaluate which ones prioritize safety alongside efficiency.
How Clinics Perform Multiple Procedures in One Day
Most Turkish clinics don’t perform one transplant per day—they’ll run three, four, or sometimes five procedures simultaneously across different operating theaters.
This isn’t reckless. It’s logistics. Each patient has a reasonable treatment time of 6–8 hours depending on graft count. While one team completes a procedure, another begins prep work with a new patient in an adjacent theater. The clinic rotates cases to keep all rooms active.
Patient safety protocols remain consistent across each room: dedicated surgeons, trained technicians, sterile equipment, and monitoring. What changes is resource allocation—clinics maximize theater use rather than leaving facilities idle between cases.
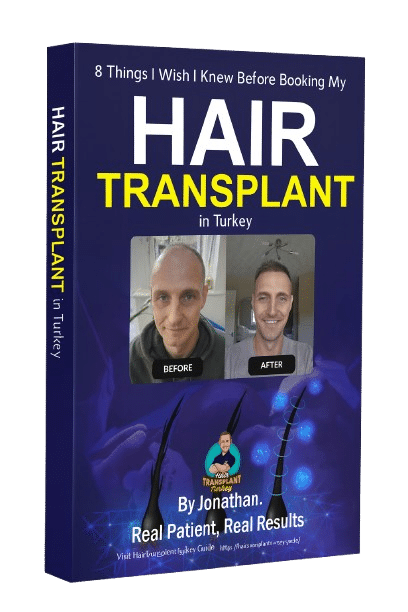
I experienced this firsthand during my January 2025 procedure at Clinicana. Other patients were being prepped and treated simultaneously, yet my care felt unhurried and focused. The system works because it’s designed around efficiency, not corners.

Staffing Models That Make High Volume Possible
To run three, four, or five procedures daily without compromising quality, Turkish clinics operate on a deliberately structured staffing model—one that’s fundamentally different from how you might expect a Western clinic to work.
The model centers on maximizing physician productivity through specialized support:
- Surgical nurses handle grafting and implantation while the surgeon focuses on extraction and design
- Technicians prepare and sort grafts in dedicated labs, eliminating bottlenecks
- Anesthetists and monitoring staff manage patient comfort across multiple operating theaters
- Coordination teams schedule procedures so surgeons move between rooms during extraction phases
This division of labor isn’t cutting corners—it’s efficient workflow strategies refined through high-volume practice. Each role is specialized, reducing idle time. When I’d my procedure, I noticed this choreography: clear handoffs, no waiting, no rushed decisions. The surgeon spent quality time on my design and extraction while trained staff managed parallel tasks.
Where Cost Savings Actually Happen (And Where They Shouldn’t)
Turkish clinics operate on margins that Western practices simply can’t match, but understanding where they actually cut costs—and where they absolutely shouldn’t—is pivotal to separating smart efficiency from dangerous corner-cutting.
The real savings come from staffing optimization, streamlined scheduling, and lower facility overhead, not from skipping steps that affect your safety or result.
I’ll walk you through each, so you can spot the difference between a clinic that’s lean and one that’s compromised.
Staff Efficiency & Scheduling
If you’ve noticed that some Turkish clinics charge half the price of others, staff scheduling is often where that gap begins—and where it can either be genuinely smart management or a red flag depending on how it’s done.
Efficient scheduling saves money through:
- Multiple surgical teams working simultaneously in separate operating theaters
- Staggered patient arrivals reducing idle time between procedures
- Technicians prepared and briefed on cases in advance
- Coordinated pre- and post-op workflows
The problem arises when efficiency sacrifices clinic patient rapport. When you’re one of ten patients processed that day, personalized experience suffers. During my January 2025 procedure, I experienced efficiency without feeling rushed—my surgical team was focused, the environment organized, yet my individual needs remained prioritized. That balance separates legitimate cost savings from corners being cut.
Clinic Infrastructure Costs
Now that we’ve looked at how clinics schedule patients, we need to examine what they’re actually spending money on—because that’s where pricing differences become both transparent and revealing.
High-volume clinics don’t cut corners on essentials. They invest heavily in operating theaters, sterilization equipment, and safety precautions that hospital regulations demand. What changes isn’t quality—it’s efficiency through scale.
When I’d my procedure at Clinicana, the hospital-based setting meant full compliance with Turkish Ministry of Health standards. That infrastructure costs money, but it’s non-negotiable.
Where clinics save isn’t safety. It’s overhead per patient. One fully equipped theater performing eight procedures daily spreads fixed costs across more surgeries than a clinic doing two. That’s why volume clinics can undercut smaller practices while maintaining identical safety standards.
Quality vs. Volume Trade-offs
Because high volume creates efficiency doesn’t mean all cost-cutting is equal. Some savings are smart; others compromise your outcome and recovery time.
Where clinics safely reduce costs:
- Streamlined scheduling and shared equipment across multiple patients
- Bulk purchasing of sterile supplies and surgical materials
- Optimized staff workflows without cutting corners on training
- Standardized protocols that maintain safety while improving speed
The problem emerges when clinics rush grafting techniques, skip individualized design work, or reduce post-operative monitoring. These create immediate cost savings but introduce long term risks—poor graft placement, infection, or inadequate aftercare follow-up.
The real question isn’t whether a clinic does 10 transplants daily. It’s whether they’re doing your transplant carefully within that volume, not despite it.
Does High Volume Mean Lower Quality Outcomes?
When you’re researching Turkish clinics, you’ll notice a stark difference in patient numbers—some facilities report doing thousands of procedures annually, while others handle a fraction of that volume. High volume disadvantages exist, but they’re not automatic. What matters is infrastructure.
A well-staffed hospital performing multiple transplants daily operates differently than an understaffed office clinic rushing patients through. Patient safety concerns arise when volume outpaces quality control—rushed consultations, assembly-line procedures, minimal aftercare. However, established clinics with dedicated teams, multiple operating rooms, and structured protocols can maintain standards at scale.
The real question isn’t volume itself, but whether the clinic has invested in systems and staffing to support it. I witnessed this firsthand—the clinic I chose handled high patient numbers without compromising attention or care protocols.
The Trade-offs Between Efficiency and Personalised Care
Once you’ve accepted that high volume doesn’t inherently mean poor outcomes, you’ll face a different question: what’re you actually willing to trade for efficiency?
High-volume clinics optimize processes, but personalised experience factors vary considerably. You might encounter:
- Shorter consultation times focused on technical assessment rather than extensive discussion
- Limited flexibility in scheduling around your specific timeline
- Less one-on-one time with your surgeon pre and post-op
- Standardized aftercare protocols rather than patient specific considerations tailored to your needs
This isn’t negligence—it’s the structural reality of scale. Some patients thrive in this streamlined environment. Others need more hand-holding and customization. Neither preference is wrong. Understanding which camp you fall into before committing helps you choose a clinic model that actually fits your expectations, not just your budget.
Red Flags That Distinguish Volume From Recklessness
When a clinic runs on assembly line economics, the pressure to move patients through the door fast can quietly become the pressure to cut corners—and that’s where volume stops being a strength and starts being a liability. I’ve seen clinics market their high case numbers like it’s a badge of honor, but what matters is whether they’re hitting those numbers because they’re genuinely efficient or because they’re skipping steps that shouldn’t be skipped.
The difference between sustainable high volume and reckless high volume comes down to what gets sacrificed when time is money.
Assembly Line Economics
Turkish clinics don’t hide their volume—they advertise it. What you’re seeing when a clinic claims 10+ daily procedures isn’t necessarily recklessness; it’s surgical throughput optimization built into their operating model.
Here’s how the economics work:
- Multiple operating theaters running simultaneously with rotating surgical teams
- Staffing productivity metrics that justify higher surgeon-to-patient ratios
- Procedural standardization reducing setup and breakdown time
- Patient scheduling designed around OR availability, not surgeon preference
The critical distinction: high volume can coexist with quality when infrastructure, regulation, and surgeon expertise support it. Hospital-based clinics with certified operating rooms and documented outcomes handle volume differently than single-room practices.
The question isn’t whether they’re busy—it’s whether their systems protect quality under pressure.
Medical Corners Cut
Just because a clinic runs multiple operating theaters doesn’t mean it’s protecting patient safety under pressure—and that’s where you need to look closest.
Red flags emerge when volume breeds insufficient oversight. Watch for: surgeons rotating between theaters without adequate rest, technicians rushing graft handling, or skipped pre-op assessments. Ethical considerations matter here. A high-volume clinic can maintain standards through proper staffing and protocols. A reckless one cuts corners on preparation time, aftercare follow-ups, or complication tracking.
When I’d my transplant, I noticed structured handoffs between teams and documented pre-op testing. That’s the difference. Ask prospective clinics directly: How many procedures per surgeon daily? Who monitors graft quality under time pressure? What’s your complication rate?
Volume isn’t the problem. Corners are.
How to Evaluate a Clinic’s Capacity Without Assuming Volume Is Bad
One of the most persistent myths in hair transplant forums is that high-volume clinics can’t deliver quality results.
The reality’s more nuanced. What matters isn’t how many procedures a clinic performs daily, but *how* they’re structured. Here’s what I evaluate:
- Staffing model: Do they’ve dedicated teams per procedure, or does one surgeon oversee multiple rooms simultaneously?
- Detailed patient timeline: Are consultations rushed, or do they allow adequate assessment and planning?
- Risk assessment considerations: How do they handle complications across high caseloads?
- Equipment and infrastructure: Can they maintain sterility and quality at scale?
Volume becomes problematic only when corners get cut—not when systems are designed to handle it. A well-organized clinic performing 10 procedures daily can outperform a smaller one doing three.
Frequently Asked Questions
If a Clinic Does 10+ Transplants Daily, How Do Surgeons Maintain Focus and Precision by Procedure 7?
Honestly? They often don’t. By procedure seven, surgeon fatigue becomes real, and patient safety concerns mount. I’d question whether focus remains sharp enough for precision work—this is why I prioritized clinics doing fewer daily procedures.
Are Patients at High-Volume Clinics Rushed Through Consultations Compared to Lower-Volume Surgeons?
You’ll often find longer consultation periods at lower-volume clinics, but don’t assume high-volume means rushed. I’ve seen both models deliver thorough assessments—what matters is whether you’re getting genuine surgeon input, not reduced patient-surgeon rapport due to time pressure.
What Happens if Complications Arise During a Busy Day—Does Volume Affect Response Time?
I’ll be honest: when you’ve got increased patient volumes, your response time matters less than whether the clinic has protocols in place. Complications don’t wait for schedules—but understaffed teams risk compromised postoperative care. That’s where structure, not just surgeon skill, counts.
Can I Request a Specific Surgeon at a High-Volume Clinic, or Am I Assigned Whoever’s Available?
You can usually request a specific surgeon, but availability depends on the clinic’s schedule. I’d recommend asking about their surgeon qualifications during consultation and checking patient satisfaction surveys—they’ll show you who consistently delivers results.
How Do High-Volume Clinics Handle Revision Cases or Patients With Complex Hair Loss Patterns?
I’ll be direct: high-volume clinics often struggle with revisions. You need a surgeon who specializes in evaluating scalp laxity and minimizing donor depletion—skills that require time, not speed. This is where volume-based models genuinely underperform.
Conclusion
You’ll find that high volume doesn’t inherently mean poor quality—it reflects smart business strategy. Turkish clinics succeed by separating surgical expertise from technical execution, allowing surgeons to focus on graft design while teams handle preparation in parallel. What matters is whether the clinic maintains rigorous safety protocols and personalized patient assessment. You can distinguish efficient scaling from corner-cutting by checking credentials, complication rates, and whether consultations feel rushed.

 Continue with Google
Continue with Google