I want to be straightforward with you: not everyone’s a good fit for hair transplants in Turkey. If you’re in your twenties or thirties experiencing unpredictable hair loss, you might think you’re ready for a procedure. But here’s what you need to know before you decide—because there’s more to candidacy than simply wanting thicker hair.
How Medical Candidacy Works for Hair Transplants
Because hair transplants aren’t cosmetic procedures in the traditional sense—they’re surgical interventions that remove living tissue from one area and relocate it to another—there are real medical criteria that determine whether you’re a suitable candidate.
Your doctor isn’t being cautious for marketing reasons. They’re evaluating whether your scalp can actually support the procedure. This means analyzing donor hair density, skin elasticity, and your body’s ability to heal without complications. Surgical scar visibility matters here—if your skin doesn’t heal cleanly, results suffer.
Your overall health, medication history, and commitment to hair regrowth maintenance also factor in.
Candidacy isn’t about age or how much hair you’ve lost. It’s about whether your biology can deliver the outcome you want.
Young Age and Unpredictable Hair Loss Progression
If you’re in your early twenties or thirties and losing hair, a transplant might feel like the obvious solution—but it’s actually one of the highest-risk decisions you can make at that stage.
Your hair loss pattern isn’t stable yet. You might be shedding due to stress, medications affecting hair growth, nutritional deficiencies, or early androgenetic alopecia that’ll progress unpredictably over the next decade. Transplanting hair now could leave you with mismatched density or an unnatural appearance as surrounding hair continues thinning.
Clinics in Turkey won’t transplant into active, diffuse loss for this reason. Before considering surgery, you need years of documented stability. Rule out treatable causes first—excessive sun exposure, hormonal imbalances, or medication side effects—and try medical treatments like minoxidil or finasteride.
Age alone isn’t disqualifying. Stability is.
Diffuse Thinning: Why Dense Donor Hair Matters
If you have diffuse thinning—where hair loss spreads across your entire scalp rather than concentrating in specific areas—a transplant becomes exponentially harder to pull off, and here’s why: the surgeon’s working with a donor area that’s already compromised.
When your donor zone doesn’t have dense, healthy hair to harvest from, you’re limited in how many grafts you can safely extract, which means fewer hairs to redistribute where you need them most. This supply constraint is the real barrier that stops diffuse thinning from being a good transplant candidate, not whether the procedure itself is technically possible.
The Donor Supply Problem
Most people don’t realise that a hair transplant’s success isn’t determined by how much hair you’ve lost—it’s determined by how much hair you’ve got left to harvest.
If you have diffuse thinning across your entire scalp, your donor area is compromised. You’re working with less dense hair to redistribute. This creates a real problem:
- Donor depletion risk – extracting too many grafts from weak donor zones leaves you visibly thinner at the back and sides
- Poor coverage results – transplanted hair can’t compensate for insufficient density in the recipient area
- Limited future options – you’ve exhausted your supply for revision work
The math is brutal. If your donor density is already low, a transplant can actually worsen your overall appearance by robbing Peter to pay Paul. That’s why honest clinicians sometimes recommend *against* surgery rather than push forward into a losing strategy.
Why Density Matters Most
The donor supply problem boils down to one thing: you can’t transplant hair you don’t have.
Density is what separates a viable candidate from a poor one. If your donor area has thin, sparse hair—what surgeons call diffuse thinning—there’s simply less usable material to work with. You might’ve enough hair on your head overall, but if it’s spread too thin across the back and sides, a transplant won’t deliver noticeable results.
Dense donor hair means thicker strands in a concentrated area. This gives surgeons grafts worth transplanting. It also reduces scalp laxity concerns—the tightness of your scalp affects how many grafts can be extracted safely.
Poor donor hair quality creates a ceiling on what’s possible, regardless of your expectations or the surgeon’s skill.
Unrealistic Expectations About Timeline and Results
When does a hair transplant actually start working? Most people severely underestimate the timeline, and that’s when candidacy breaks down.
If you’re expecting visible results in three months, you’ll likely feel disappointed—even if the procedure’s technically successful. Here’s what unstable expectations look like:
- Assuming transplanted hair grows immediately (it doesn’t; shedding occurs first)
- Believing one session creates a full, natural head of hair (often two procedures are needed)
- Overlooking limitations of your donor supply or scalp laxity
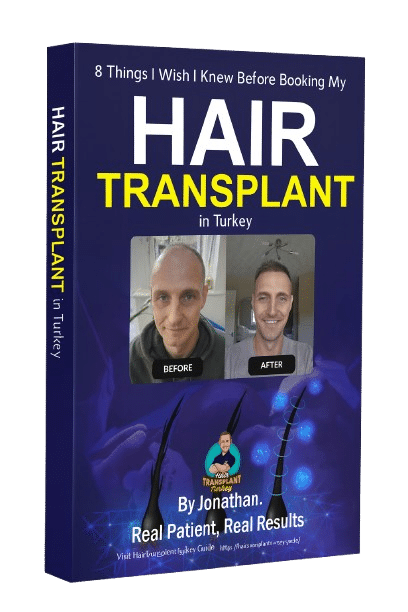
I didn’t see meaningful regrowth until month four, with strong results by month six or seven. That’s normal. But if you can’t psychologically handle that waiting period—or you’re hoping for a miracle—you’re not ready yet. Patience isn’t optional; it’s part of the process.
Unstable Health or Uncontrolled Medical Conditions
If you’re managing a blood clotting disorder or uncontrolled diabetes, a hair transplant isn’t a safe procedure to pursue right now—and here’s why. Both conditions directly affect your body’s ability to heal properly: clotting disorders increase bleeding during and after surgery, while uncontrolled diabetes compromises wound healing and infection resistance.
Getting your health stable first isn’t just recommended—it’s essential before any surgical intervention.
Blood Clotting & Bleeding Disorders
Blood clotting disorders and bleeding conditions represent a genuine medical contraindication for hair transplantation—and it’s one where honesty matters more than reassurance.
Hair transplants involve controlled bleeding and require precise hemostasis (blood clotting) during and after surgery. If your body can’t clot properly, you face real risks:
- Excessive bleeding during the procedure that’s difficult to control
- Prolonged oozing and hematoma formation post-op, compromising graft survival
- Infection risk from unhealed extraction and implant sites
Conditions like hemophilia, von Willebrand disease, or thrombocytopenia disqualify you outright. Similarly, medications interfering with clotting—anticoagulants, certain NSAIDs, blood thinners—create unsafe surgical conditions.
Your surgeon will screen for these blood-related conditions during consultation. If you have a known bleeding disorder, don’t pursue this procedure in Turkey or elsewhere. The cosmetic goal isn’t worth the medical risk.
Diabetes & Wound Healing
Beyond blood-related contraindications, uncontrolled metabolic conditions like diabetes create equally serious barriers to safe hair transplantation.
Your body needs stable blood sugar and healthy wound-healing capacity to close these sites properly and resist infection.
Uncontrolled diabetes impairs both. High glucose levels slow healing, weaken immune response, and increase infection risk—complications that can compromise graft survival and leave visible scarring.
Thyroid disorders present a similar concern. An unstable thyroid affects metabolism, immune function, and tissue repair, all critical during recovery.
If you have diabetes or thyroid issues, it doesn’t automatically disqualify you. But your condition must be well-managed, documented, and cleared by both your regular physician and the transplant surgeon. This isn’t negotiable.
Poor Access to Aftercare and Follow-Up Support
A hair transplant doesn’t end when you leave the clinic—it’s the months afterward that determine whether your investment delivers real results.
If you can’t access consistent follow-up support after returning home, you’re at genuine risk. Remote aftercare matters because:
- Surgical complications (infection, poor healing) need prompt identification and guidance
- Lack of follow-up communication leaves you uncertain about normal recovery versus warning signs
- Graft care instructions require clarification as your scalp evolves through healing phases
When I’d my procedure in Istanbul, aftercare continued via structured WhatsApp check-ins after I returned home. That ongoing contact gave me confidence when questions arose.
If your chosen clinic offers only pre-procedure support, reconsider. You need accessible, responsive aftercare—whether remote or local—throughout your first year.
Frequently Asked Questions
Can I Get a Hair Transplant if I’m Taking Medications That Affect Hair Loss?
Yes, you can often get a transplant while taking hair-loss medications, but I’d recommend disclosing all medications to your surgeon. They’ll assess potential medication interactions and underlying medical conditions to verify you’re a safe candidate.
What Happens if My Donor Hair Starts Thinning After My Transplant?
Your transplanted hair won’t thin—it’s genetically resistant. However, if your donor hair quality deteriorates from ongoing hair loss, future transplants won’t restore lost density. That’s why I recommend stabilizing your hair loss before surgery.
Is Hair Transplant Success Affected by Ethnicity, Hair Type, or Curl Pattern?
Your ethnicity and curl pattern don’t determine transplant success—genetic hair loss causes do. I’ve seen excellent results across all hair types. What matters is whether your donor supply can sustain regrowth, regardless of curl pattern differences.
How Do I Know if My Hair Loss Is Stable Enough for Surgery?
You’ll know your hair loss is stable when you haven’t experienced noticeable progression over 6-12 months. Your surgeon assesses this during consultation—checking your hair loss pattern, scalp laxity, and whether you’re still actively shedding.
Can Financial Constraints Delay My Aftercare and Still Achieve Good Results?
I’d say no—skipping aftercare won’t give you the results you paid for. A limited budget shouldn’t delay your extended recovery period. Plan for full aftercare costs upfront, or delay surgery until you can afford both the procedure and proper follow-up care.
Conclusion
You shouldn’t rush into a hair transplant if you’re young with unpredictable hair loss, have diffuse thinning, or expect instant results. I’d urge you to wait until your hair loss stabilizes, guarantee you’ve got realistic expectations about the 4-7 month recovery period, and confirm you can access proper aftercare. A successful transplant requires the right candidate—not just the right surgeon.

 Continue with Google
Continue with Google