I’ve found that most people considering a hair transplant focus solely on their first procedure—but that’s where many get blindsided. Your donor supply isn’t infinite, and how you approach that initial transplant directly shapes what’s possible down the road. If you’re dealing with progressive hair loss, you’ll want to understand something critical about spacing, density, and long-term planning. Let me walk you through what actually matters.
How Much Donor Hair Do You Actually Have, and Can It Run Out?
Unless you’ve looked at your own scalp under a microscope, you probably don’t know how many follicles you’re working with—and that’s exactly why this question matters before you commit to a transplant.
Your donor size estimation depends on several factors: scalp laxity (how loose your skin is), hair density, and follicle characteristics. A surgeon evaluates these during consultation to determine your safe extraction limit—typically between 4,000 and 10,000 grafts, though some people have considerably more.
Yes, donor hair can theoretically run out, but it’s rare if you’re realistic about planning. The key is understanding your donor hair quality assessment upfront. This prevents the frustrating scenario where you’ve exhausted your supply but still have visible hair loss.
Why a Second Hair Transplant Isn’t Always the Obvious Choice
So you’ve got 6,000 grafts available, you’ve used 5,000 in your first transplant, and you’re thinking: why not just do another round with what’s left?
It’s logical, but not always smart. Here’s why:
- Diminishing returns on small graft counts — 1,000 grafts won’t meaningfully address permanent hair loss across your scalp; you’ll see minor density improvement at best.
- Increased donor area trauma — A second procedure stresses the same limited zone, raising scarring risk and compromising future suitability for transplant.
- Medical vs. cosmetic timing — Your first result needs 12–18 months to fully mature. A second transplant during this window can obscure what you actually gained.
Reserve remaining grafts for strategic touch-ups later, not reflexive second procedures.
Timing Your Next Procedure: What the Research Says About Waiting Periods
If you’re considering a second transplant, you need to understand three critical constraints: how long your scalp actually needs to heal, how much donor hair you can safely harvest, and what happens to density when you go back for more.
I’ll walk you through what the research actually says about spacing procedures, because the timeline matters far more than clinic marketing suggests.
Minimum Safe Waiting Periods
Many people who’ve had one hair transplant eventually consider a second—whether to densify existing results, address new hair loss, or extend coverage to areas they couldn’t afford initially.
The research is clear: adequate resting periods between procedures protect your donor supply and guarantee sustained growth projections from your first transplant.
- Wait 12 months minimum – This allows your first transplant to fully mature and stabilize, typically by month 9–12.
- Assess real density gains – You can’t accurately plan a second procedure until you’ve seen your actual results; premature planning leads to miscalculation.
- Preserve donor integrity – Harvesting again too soon increases scarring risk and compromises future options.
Most surgeons recommend spacing procedures 18–24 months apart. This isn’t arbitrary—it’s based on healing cycles and donor regeneration.
Donor Depletion and Density Loss
Every hair you harvest from your donor area—typically the back and sides of the scalp—represents a finite resource that won’t regenerate. This reality shapes everything about long-term transplant planning.
Your donor supply isn’t unlimited. Most people have between 4,000 and 7,000 harvestable grafts. Once extracted, those follicles are gone permanently. This creates real donor exhaustion concerns if you pursue multiple procedures without understanding your limits.
Hair density fluctuations also matter. After your first transplant, density in the donor zone decreases slightly. A second procedure harvests from an already-thinner area, which can look noticeable if you wear your hair short.
The practical takeaway: know your total graft budget before committing to a second transplant. This isn’t doom—it’s planning.
Scalp Healing and Scar Maturation
Your scalp doesn’t finish healing immediately after surgery. Full maturation takes months, and understanding this timeline matters if you’re planning a second procedure.
Scar visibility peaks early — donor and recipient sites look most prominent at 4–6 weeks, then gradually fade as collagen remodeling continues for up to 18 months.
Pigmentation changes occur gradually — redness subsides over 3–4 months as inflammation settles, but deeper pigmentation matching can take longer.
Tissue stabilization requires patience — waiting 12–18 months between procedures allows scars to mature fully, giving surgeons clearer visibility of viable donor density and better recipient site assessment.
Rushing a second transplant before your scalp fully heals increases scar visibility and compromises surgical precision. This is why most surgeons recommend waiting at least a year between procedures.
Maximizing Donor Supply Across Multiple Transplants: Density, Placement, and Strategy
If you’re planning multiple transplants, you can’t just extract grafts wherever they’re available—you need a deliberate strategy that preserves donor density and accounts for future procedures. The way your surgeon places grafts in your first transplant, and how aggressively they harvest from your donor zone, directly determines what options you’ll have for a second or third procedure down the line.
We’ll walk through how density distribution, donor preservation, and procedural sequencing actually work together to maximize your long-term outcomes.
Strategic Density Distribution
One of the most misunderstood aspects of hair transplant planning is density—specifically, how many grafts a surgeon can place in a given area, and what that means for long-term strategy across multiple procedures.
A thoughtful hairline design doesn’t maximize density everywhere. Instead, it distributes grafts strategically:
- Front line priority — Higher density at the hairline creates definition; lower density behind preserves donor supply for future needs
- Density pattern progression — Density naturally decreases moving backward, mimicking how hair actually grows
- Temporal zones — Temples use fewer grafts per square centimeter than the crown, allowing flexibility for second procedures
This graduated approach means you’re not exhausting your donor supply on your first transplant. You’re building a multi-decade plan that accounts for aging and potential future hair loss patterns.
Donor Site Preservation Methods
Because density decisions made during your first procedure directly impact what’s available for your second, third, or even fourth transplant, donor site preservation isn’t an afterthought—it’s the backbone of long-term planning.
Your surgeon should never extract every available graft. Instead, they’ll preserve donor density by using conservative extraction rates—typically 4,000–5,000 grafts per procedure rather than the maximum possible. This approach keeps your scalp looking natural long-term and leaves reserves for future work.
If you’re considering strip surgery, understanding strip scar aesthetics matters: a well-placed linear scar can be concealed and theoretically revised, but it does consume donor area. FUE avoids this but requires more time and precision.
The goal’s simple: look good now and tomorrow.
Planning For Future Procedures
Most people think about their hair transplant as a single event—you get the procedure, you wait for results, and you’re done.
Reality’s different. If you’re younger or experiencing aggressive hair loss patterns, you’ll likely need a second procedure within 5–10 years. Planning ahead changes everything.
Strategic grafting during your first transplant matters enormously. Your surgeon should consider:
- Preserving donor density for future extractions without visible depletion
- Placing grafts strategically to accommodate your evolving hair loss patterns
- Using advanced restoration techniques that maximize coverage while minimizing waste
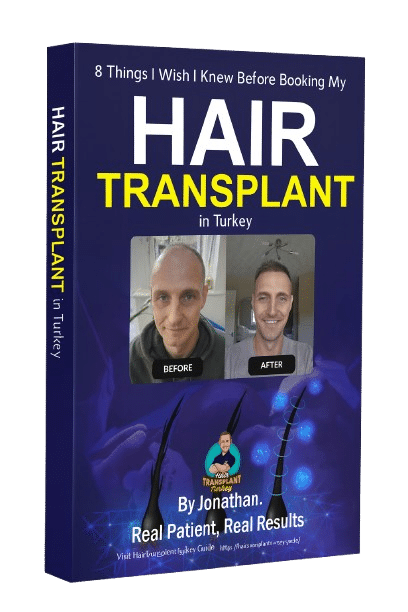
When I’d my procedure, my surgeon mapped my likely progression and spaced grafts thoughtfully—not just filling current gaps. This foresight means I’m not locked into one outcome. Instead, I’ve got genuine options for what comes next, whether that’s touch-ups or fuller restoration.
What Happens to Transplanted Hair After 10 Years: and Beyond
Hair transplants aren’t a one-time event with a fixed expiration date—they’re a long-term investment that evolves over decades. Transplanted hair, taken from genetically resistant donor zones, typically remains stable for 10+ years and often indefinitely. However, your native hair continues thinning, which shifts crown density considerations and overall appearance over time.
By year 10, you’ll likely notice the transplant’s relative prominence increase as surrounding hair thins further. This creates practical planning decisions: accepting the gradual shift, pursuing a second procedure, or exploring medical options like finasteride to slow native loss.
Scalp laxity and follicular yield—your remaining donor supply—become critical factors if you’re considering future transplants. Repeated procedures reduce available donor tissue, making earlier procedures strategically important to maximize your lifetime follicular yield before options narrow.
Building a Realistic Long-Term Plan With Your Surgeon
If you’re thinking beyond your first transplant, the surgeon’s role shifts from technician to strategist.
A good surgeon doesn’t just harvest and implant—they map your lifetime needs. This means:
- Discussing expectations for long-term growth across different scalp zones and how density might change over decades
- Managing your hopes and fears by being honest about donor limitations and realistic timelines rather than overpromising density
- Planning staged procedures if you’re young or have aggressive hair loss, spacing transplants strategically to preserve remaining donor supply
During my consultation, this forward-thinking approach mattered more than the pitch. The surgeon asked about my family history, lifestyle, and what I’d accept if results plateaued. That conversation shaped everything—not just the first procedure, but how I’d approach any future work.
Frequently Asked Questions
Can Body Hair Be Used as a Donor Source if Scalp Supply Runs Low?
Yes, body hair—particularly beard hair—can supplement scalp donor supply, though it grows slower and requires careful donor site considerations. I’d recommend discussing realistic expectations about growth rate and timeline with your surgeon before pursuing this option.
Does Transplanted Hair Eventually Turn Grey at the Same Rate as Original Hair?
Yes, transplanted hair grays at the same rate as your original hair because it retains your donor genetics. The gradual graying rate you’ll see depends on your ethnic hair pigmentation differences and your family’s aging patterns.
What Happens if I Lose More Hair After My First Transplant Procedure?
If you lose more hair after your first transplant, you’ve got options. I’d recommend planning a second procedure once you’ve stabilized—typically 12-18 months later. That’s when increased shedding settles, and you’ll see your true donor supply remaining for future procedure planning considerations.
Are There Non-Surgical Options to Stretch Donor Supply Between Transplant Sessions?
Yes. Topical treatments like minoxidil and finasteride can slow hair loss and preserve remaining donor hair between procedures. They’re your best non-surgical option to maximize what you’ve got before considering surgical alternatives later.
How Do Age and Genetics Affect How Many Transplants I Can Realistically Have?
Your age and genetics fundamentally determine how many transplants you’ll realistically get. I’d assess your familial hair follicle density and generational hair loss patterns—these show how much donor supply you’ve inherited and how aggressively your hair’ll thin over time.
Conclusion
You’re working with a finite donor supply, so planning strategically matters more than rushing into multiple procedures. By spacing transplants at least 12 months apart and focusing on smart placement rather than maximum density, you’ll preserve your options for future needs. Partner with your surgeon to build a realistic roadmap that sustains your results for decades, not just the next few years.

 Continue with Google
Continue with Google