Understanding the hair transplant recovery timeline isn’t just about managing expectations—it’s about recognizing the complex biological processes that determine your final results. After undergoing hair restoration surgery in Istanbul at Clinicana, I discovered that the journey from procedure to full results involves far more than simply waiting for hair to grow. The science behind graft survival, growth cycles, and recovery phases reveals why patience and proper care are essential for optimal outcomes.
Understanding the Hair Growth Cycle: The Foundation
Before diving into the transplant recovery timeline, it’s crucial to understand how hair naturally grows. Hair follicles cycle through four distinct phases: anagen (growth), catagen (transition), telogen (rest), and exogen (shedding).
The anagen phase is the longest, lasting approximately two to eight years for scalp hair, during which the hair shaft actively grows from the follicle. In a healthy scalp, approximately 85-90% of hairs are in the anagen phase, 1-2% in the catagen phase, and 10-15% in the telogen phase at any given time. Recent research challenges the traditional assumption about these percentages—one study found a higher percentage of scalp follicles in catagen (7.5%) than in telogen (3.5%), suggesting our understanding of hair cycling continues to evolve.
The telogen phase typically lasts around 2-3 months before the hair is shed and a new anagen phase begins. This natural cycling is central to understanding what happens after a transplant.
Day 1: The Critical First Hours
On the first day post-surgery, my scalp was cleaned at the clinic, and I received detailed instructions on proper washing and care techniques. The first few days after a hair transplant procedure are the most critical, as hair follicles must adapt to their new environment. Under typical conditions, neovascularization—the formation of new blood vessels—begins within 2 to 5 days post-transplantation. These initial days set the foundation for graft survival.
During this period, maintaining proper hygiene while protecting vulnerable grafts is paramount. The grafts need to establish connections with the surrounding tissue and blood supply to survive.
Week 1-2: Healing and Scab Formation
The first two weeks represent what clinicians call the “initial recovery period.” During this time, small incisions made by the surgeon take time to scab over, and patients must minimize the chances of infection while the scalp heals.
Swelling is a natural reaction to surgery, often appearing on the forehead and around the eyes, caused both by tissue trauma and fluids injected during the procedure for local anesthesia. In my case, scabs formed around each transplanted graft—a normal part of healing. By around 7-10 days post-surgery, the transplanted grafts build strength and are less likely to fall out when touched.
By day 7, most scabs should be gone, leaving the scalp slightly pink. This is when many patients feel confident enough to return to work, though the most dramatic phase is just beginning.
Week 3-4: The Shocking Truth About Shock Loss
Around weeks 2-4 came the most psychologically challenging phase: shock loss. Most of my transplanted hairs fell out during this period. This wasn’t a failure—it was expected biology.
Shock loss happens because transplanted follicles often go into the telogen phase and release the hair shaft. The surgical trauma causes the grafts to enter a resting state. I remember looking in the mirror at 4 weeks and seeing mostly clean scalp where the new hairline had been. This phase tests patience, but understanding the science makes it bearable.
Approximately 4-5 days after the procedure, newly transplanted hair in the recipient area begins to shed, with the hair shafts falling out while the implanted follicles remain safely embedded in the scalp. Clinical data confirms this universal experience, with most patients experiencing significant shedding between weeks 2-4.
Month 2-3: The Waiting Game
Once hair has shed, follicles enter the telogen resting phase, which takes about 2 to 2.5 months. During these months, little visible growth occurs. The follicles are metabolically active beneath the surface, preparing to restart their growth cycle, but externally, progress seems minimal.
This period requires the most patience. Friends and family may ask about results, but there’s little to show. The transplanted area looks similar to how it did immediately after shock loss—clean, with minimal visible hair.
Month 3-6: Early Growth Emerges
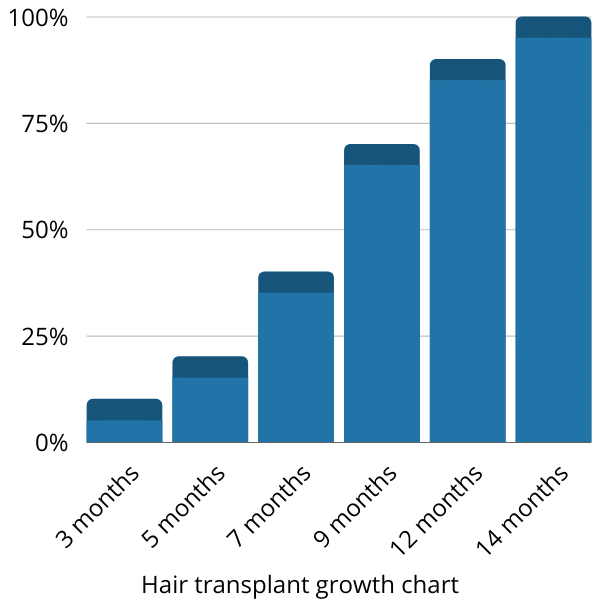
By month 3, I began seeing tiny sprouts of new hair—what I called “baby hairs”—poking through the scalp. Clinical observations show initial growth becomes visible at 3 months and reaches approximately 20% of final fullness by month 5.
Around the beginning of the 4th month after transplant, new hair begins to grow, initially appearing thin and potentially curly before thickening and straightening as it grows longer. By month 3-4, I could confirm the grafts had survived and were producing new hair, even though coverage remained sparse.
By month 6, the transformation became more apparent. Coverage jumped significantly—roughly half of the final fullness was visible. Many sources note that after 4-6 months, grafts thicken noticeably, often reaching 50-80% of eventual density by month 6. This is when most patients start feeling genuinely excited about their results.
Month 6-9: The Growth Spurt
The biggest improvement generally occurs between the 5th and 9th months. During this period, my hair felt increasingly fuller and denser with each passing week. The transplanted hairs were not only growing longer but also thickening, which contributed significantly to overall coverage.
Between 5-8 months, the majority of follicles grow hairs again, with regrowth becoming more uniform. This phase is visually rewarding after the long wait. Friends who hadn’t seen me since the surgery noticed obvious improvements.
Month 12-18: Achieving Final Results
The NHS confirms that by 12 months, most growth (around 90%) is achieved, with final maturation occurring up to 18 months. Charts from hair clinics suggest approximately 90% density by 12 months and true 100% by 14-18 months.
My own photos at month 12 showed nearly all the transplanted hair had grown in, matching clinical predictions. The Mayo Clinic predicts “best results” at 8-12 months, though subtle improvements continued beyond the one-year mark.
By 18 months, the transplanted hair had reached its full potential—both in terms of density and thickness. The waiting period, while challenging, ultimately delivered results that met the clinical averages.
Complete Timeline Summary
Here’s the comprehensive recovery timeline based on both personal experience and clinical data:
Day 1: Scalp cleaned professionally; grafts in place; neovascularization beginning
Week 1-2: Scabs form and begin falling off; swelling and redness improve; grafts strengthen
Week 3-4: Scabs mostly gone; shock shedding of transplanted hairs begins (expected and normal)
Month 2-3: Resting phase; minimal visible growth; follicles preparing beneath the surface
Month 3-6: New hair starts growing (approximately 10-20% fullness by month 3-4, reaching 50-80% by month 6)
Month 6-9: Rapid thickening; most growth achieved; visible transformation occurs
Month 12-15: Hair reaches approximately 90-100% of full length and density
Month 12-18: Final maturation; subtle continued improvements
Graft Survival Rates: What the Data Shows
One of the most important questions is: how many transplanted grafts actually survive? Currently, hair transplants have between a 95-98% success rate on average. This high survival rate occurs because the hair follicles come from the patient’s own scalp, eliminating rejection risk.
However, survival rates vary depending on the technique used. For FUE (Follicular Unit Extraction) transplants like mine, published studies report over 90% of grafts surviving at one year, with a recent study of 158 men finding mean follicle survival of approximately 91% at 1-2 years. FUT (Follicular Unit Transplantation or “strip method”) often reports similarly high survival rates around 95%.
Some early studies found lower survival rates for FUE grafts compared to FUT (53.9% vs 85.2%), though other research found survival of FUE grafts equivalent to that of FUT grafts. The discrepancy often relates to surgeon skill, technique refinement, and graft handling. Modern FUE techniques have dramatically improved outcomes compared to early methods.
The International Society of Hair Restoration Surgery released a study in 2018 comparing success rates of the two hair transplant methods, finding both performed equally well within all parameters, with FUE performing slightly better in some ways.
Density Considerations
Clinical data indicate near-complete survival at densities of 30 grafts/cm², but this rate declines to approximately 84% at 50 grafts/cm². Dense packing can increase ischemia risk—when grafts compete for blood supply, some may fail to thrive. This highlights why experienced surgeons carefully plan graft placement to balance density with survival.
Factors Affecting Your Personal Timeline
While the timeline above describes average experiences, individual results vary significantly. Understanding the factors that influence your recovery helps set realistic expectations.
1. Genetics and Baseline Hair Characteristics
Family history of baldness largely determines how your native and transplanted hair will fare. Transplants don’t stop genetic balding, so someone prone to heavy balding may continue losing untreated areas even after a successful transplant.
Fine, sparse, weak donor hair often results in poor coverage and poor survival. Hair texture, thickness, and density all influence final appearance. Patients with thick, dense donor hair typically achieve more dramatic visual improvements than those with fine, sparse hair.
2. Surgical Technique and Clinic Quality
Meticulous handling, including keeping grafts moist and careful placement, can boost survival. The surgeon’s experience significantly impacts outcomes. The best hair transplant surgeons have transection rates of 5% or less, while less capable surgeons can have transection rates between 20-75%.
Loss of grafts to dehydration has been documented in several studies, with reported survival time in a dry environment ranging from 3 minutes to greater than 16 minutes before significant graft death occurs. Proper graft handling during the brief time outside the body is critical.
The surgical team’s expertise in creating recipient sites, placing grafts at proper angles, and maintaining appropriate density all influence long-term results. This is why choosing a reputable clinic with experienced surgeons matters tremendously.
3. Aftercare and Patient Compliance
Proper aftercare significantly influences graft survival and growth quality. Following my clinic’s instructions carefully—sleeping semi-upright, avoiding harsh contact with grafts, using gentle shampoo techniques—helped ensure optimal healing.
Aftercare instructions typically include keeping the head elevated while sleeping to reduce swelling, applying cold compresses to the forehead to help reduce swelling and discomfort, and following specific guidelines on when and how to wash hair.
Discontinuing antiplatelet and anticoagulation medications before hair transplantation can help mitigate bleeding risk. Patients should discuss all medications with their surgeon before the procedure.
4. Nutrition and Overall Health
Hair follicles are highly metabolically active and require a consistent supply of nutrients to function properly. The health of transplanted follicles relies heavily on nutrient-rich blood supply.
Iron helps transport oxygen to follicles, zinc assists in tissue regeneration and immune support, while biotin promotes keratin production. If a patient’s diet lacks these essential nutrients, it may lead to weaker hair regrowth or thinning.
Key nutrients for optimal recovery include:
- Protein: Essential for keratin production and hair shaft formation
- Iron: Supports red blood cell formation and follicle oxygenation
- Vitamin C: Assists iron absorption and collagen production
- Biotin (Vitamin B7): Strengthens keratin structure
- Vitamin D: Regulates hair growth cycle
- Zinc: Supports immune function and tissue healing
- Vitamin E: Provides antioxidant protection
A healthy diet rich in essential vitamins and minerals can help speed up the healing process and promote new hair growth. Foods particularly beneficial after transplant include lean proteins, leafy greens, citrus fruits, nuts and seeds, beans and lentils, and fatty fish.
Medical conditions such as thyroid disorders, diabetes mellitus, autoimmune conditions, infections, and nutritional deficiencies can all impact transplant results. Addressing underlying health issues before and after surgery supports better outcomes.
5. Age and Hormonal Factors
The proportion of follicles in anagen phase declines with age. Younger patients often experience faster, more robust growth than older patients, though successful transplants occur across all adult age groups.
Hormonal balance also influences results. Hormonal imbalances can affect hair growth after transplant. For male patients, DHT (dihydrotestosterone) continues to affect native hair even after transplant, which is why many surgeons recommend ongoing maintenance treatments like finasteride or minoxidil.

Why Does Full Growth Take 12-15 Months?
Understanding why complete results require such patience helps manage expectations. Scalp hair grows at approximately 0.35 mm per day, 1 cm per month, or 15 cm per year. Even after a follicle restarts the anagen phase, it needs many months to rebuild thickness and length.
Clinical guides agree: new hair often appears by about 3-4 months, with final results seen by 10-18 months post-op. The extended timeline reflects the natural hair growth cycle, not surgical failure or poor technique.
Additionally, transplanted follicles don’t all restart simultaneously. They activate at different times, which is why growth appears gradual and uneven during months 3-9. This staggered activation actually produces more natural-looking results than if all follicles activated simultaneously.
Long-Term Considerations
While 12-18 months marks the achievement of full results, long-term maintenance remains important. A study tracking patients four years after FUT found that only 8.92% of subjects retained the same density of transplanted hairs, with the rest showing various grades of reduction in density.
These findings suggest recipient-site influence might affect the growth and survival of transplanted hairs. While transplanted hairs from the “safe donor area” are genetically resistant to DHT, some thinning over years may still occur due to aging, ongoing androgenetic alopecia affecting surrounding native hairs, or other factors.
This doesn’t mean transplants fail—it means that like all hair, transplanted hair ages and may thin over time. Many patients maintain excellent results for decades, but some may eventually consider supplementary treatments or additional procedures.
Setting Realistic Expectations
My timeline—some early shock loss, mild sprouts by 3 months, and a visible new hairline by month 7—matched scientific averages. However, charts and statistics describe averages, and individual journeys may shift if you have faster or slower hair cycles.
Some patients see earlier growth, while others experience delays. Neither scenario necessarily predicts final outcome quality. Individual variations and factors such as post-transplant care can affect the success of hair growth.
While hair density can improve significantly after a successful transplant, it may not reach the same level as before hair loss, but it can still provide significant improvement in overall appearance. Understanding this helps prevent disappointment when comparing post-transplant density to one’s hair as a teenager.
Red Flags: When to Consult Your Surgeon
While patience is essential, certain signs warrant professional consultation:
- Excessive pain, swelling, or signs of infection during the first weeks
- Complete lack of growth by month 6-7 (some early growth should be visible)
- Significant patchiness or extremely uneven growth beyond month 9
- Continued heavy shedding beyond the expected shock loss phase
- Unusual redness, inflammation, or scarring that worsens rather than improves
If you’re concerned about density after 5 months of a hair transplant, consult a hair transplant specialist to determine the cause and find a solution. Most concerns have explanations and solutions, but professional evaluation provides peace of mind.
Enhancing Your Results
While you can’t dramatically accelerate the natural hair cycle, certain supportive treatments may optimize growth:
Some clinics recommend supplementary treatments including Platelet-Rich Fibrin (PRF) therapy, which uses your own blood plasma rich in growth factors to stimulate hair growth, and Low-Level Laser Therapy (LLLT), a non-invasive treatment using red light to stimulate hair follicles.
Platelet-rich plasma (PRP) therapy utilizes autologous blood-derived platelets to support tissue healing and stimulate follicular regeneration. While evidence for these therapies continues to develop, many clinics report positive results when used as adjunct treatments.
Medications like minoxidil (Rogaine) can support overall hair growth, and finasteride can help prevent further loss of native hairs. Discussing these options with your surgeon helps develop a comprehensive maintenance strategy.
Final Thoughts
Whether you’re in week 3 experiencing shock loss, month 5 seeing early sprouts, or month 9 watching dramatic improvements, knowing you’re on track when following proper post-op care routines provides reassurance.
The hair transplant recovery timeline is predictable in its general pattern but unique in individual details. Genetics, surgical skill, graft count and survival, and aftercare all influence outcomes. Understanding the biology behind the timeline—the hair growth cycle, neovascularization, and follicle activation—transforms waiting from anxious uncertainty to informed patience.
My journey from a newly transplanted hairline through shock loss to full results at 12 months followed the established clinical patterns. The data proves that while hair restoration requires time, it delivers lasting results for the vast majority of patients who choose qualified surgeons and commit to proper aftercare.
For those considering or recovering from a hair transplant, remember: patience isn’t just virtue—it’s biology. Trust the process, follow your aftercare instructions, maintain proper nutrition, and give your follicles the 12-18 months they need to deliver the full, natural-looking results you desire.
Sources and special thanks
Thanks to you, the reader, for reading this article. I hope it was useful for you. This article is based on my personal experience at Clinicana, Istanbul, combined with clinical research and studies including data from the Mayo Clinic, NHS, PubMed, and various peer-reviewed journals on hair transplant outcomes and recovery timelines.

 Continue with Google
Continue with Google