I’ve seen countless patients return from Turkey with impressive transplant results, only to watch their native hair continue thinning within months. Here’s what most clinics won’t emphasize: your transplanted grafts are protected, but your remaining hair isn’t. Whether finasteride truly matters for your outcome depends on factors your surgeon should’ve discussed before surgery. Let’s explore what actually happens when you skip it.
What Finasteride Does and Why It Matters After Hair Transplant Surgery
Because a hair transplant only moves existing hair rather than stopping hair loss, finasteride becomes relevant the moment you’re considering whether your transplant investment will last.
Finasteride works by blocking DHT, the hormone that shrinks hair follicles in genetically predisposed men. Transplanted hair is resistant to this miniaturization, but your non-transplanted hair isn’t. Without finasteride, you risk continued loss in untreated areas, creating an unbalanced result over time.
This is why transplant longevity depends partly on what happens after surgery. The grafts themselves won’t fall out, but surrounding hair loss can undermine your outcome. Strong medication adherence—taking finasteride consistently—protects both your investment and the natural appearance of your hairline as years pass.
The Critical Difference Between Transplanted Hair and Native Hair
This is where understanding finasteride’s role becomes inseparable from understanding why you’d need it in the first place.
Transplanted hair comes from your donor area—typically the back of your scalp—where hair follicles are genetically resistant to DHT, the hormone driving male pattern baldness. That resistance doesn’t change after surgery. Your transplanted hair won’t fall out due to genetics.
Your native hair, however, remains vulnerable. If you’re prone to androgenetic alopecia, the hair you were born with will continue thinning regardless of your transplant. This surgical technique consideration matters because your result depends on protecting what you still have.
Finasteride doesn’t preserve transplanted hair. It preserves your native hair requirements—the surrounding scalp that frames your transplant and determines your overall appearance long-term.
Do Transplanted Grafts Need Finasteride to Survive?
The short answer is no—transplanted hair follicles won’t fall out because you’re not taking finasteride.
Transplanted grafts come from DHT-resistant donor areas, typically the back and sides of your scalp. These follicles are genetically programmed to resist miniaturization regardless of DHT exposure. That’s the entire point of hair transplantation: moving hair that’s already resistant to the hormone causing your loss.
However—and this matters—finasteride isn’t about graft survival. It’s about protecting your remaining native hair. Your non-transplanted follicles may still be vulnerable to DHT. Without medication resistance built in, they’ll continue thinning if you’re genetically predisposed.
Think of it this way: your transplant is protected. Your original hair isn’t. Finasteride addresses that gap, not graft quality control.
When Does Finasteride Actually Become Important Post-Transplant?
they assume finasteride matters immediately after surgery, so they either rush to start it or worry about missing a critical window.
The truth is simpler. Transplanted grafts don’t need finasteride to survive—they’re genetically protected. What matters is your native hair. If you’re losing it, finasteride becomes important around month 3–4 post-transplant, when your medication needs align with your recovery timeline and surgical considerations allow stable dosing.
Starting finasteride before surgery or during the first few weeks creates unnecessary medication complications during healing. Most clinics recommend waiting until initial recovery’s complete, then beginning if you have active hair loss elsewhere on your scalp.
The timing isn’t about saving grafts. It’s about stopping further loss in untreated areas.
Common Concerns: Side Effects, Timing, and Who Should Avoid It
By now you’re probably wondering whether finasteride is right for you—and honestly, that concern makes sense, because it’s not a one-size-fits-all answer.
The reality is that side effects are real for some people, timing matters, and there are specific situations where you shouldn’t take it at all.
Let’s break down what actually matters and what’s just noise.
Finasteride And Native Hair
While finasteride’s role in preserving your transplanted hair is straightforward, its effects on your native hair deserve equal attention—and they’re where most patients’ real concerns actually lie.
Finasteride works by blocking DHT, the hormone driving genetic hair loss. If you’re experiencing androgenetic alopecia, it can slow or halt hair loss in your non-transplanted areas. That’s the protective benefit most people overlook.
However, medication safety requires realistic expectations. Finasteride isn’t a cure—it maintains what you have. Results vary considerably between individuals. Some see substantial stabilization; others see minimal change.
The lifestyle adjustments matter too. Consistency is everything. Stopping finasteride typically reverses its protective effects within months, so it’s a long-term commitment if you choose it. Discuss your specific hair loss pattern with your surgeon before deciding whether finasteride aligns with your goals.
Side Effects: What’s Real
The conversation around finasteride’s side effects often spirals into fear-based narratives that don’t match the clinical reality. Yes, sexual dysfunction and reduced libido are documented in clinical trials—but they occur in roughly 2% of users, and often resolve after discontinuation.
What matters more is understanding potential interactions with other medications and committing to long term compliance. If you’re already taking blood pressure medication or other prescriptions, mention finasteride to your doctor first.
The real risk isn’t the side effects themselves—it’s stopping suddenly after seeing results. Hair transplants work best when your native hair stays protected. That requires consistency, not perfection. Most men tolerate finasteride well. Your individual health history determines whether it’s right for you.
Medical Contraindications And Alternatives
Not everyone should take finasteride, and that’s where the conversation needs to shift from side effects to actual medical safety.
You shouldn’t use finasteride if you have:
- A history of prostate cancer or elevated PSA levels without medical clearance
- Liver disease or severe kidney impairment affecting drug metabolism
- Known hypersensitivity to finasteride or dutasteride
Your surgeon should review your full medical history before recommending it. Differing surgical techniques—like FUE versus FUT—don’t change whether finasteride suits you medically.
If finasteride isn’t an option, alternatives exist: minoxidil (topical or oral), low-level laser therapy, or maintaining realistic expectations about transplant stability alone. Some men choose no medication at all, understanding that transplanted hair won’t fall out, but native hair loss may progress differently.
The key: medical contraindications trump marketing claims every time.
What the Research Actually Shows About Long-Term Outcomes
Most conversations about finasteride after a hair transplant rest on assumptions rather than evidence, so it’s worth breaking down what the research actually demonstrates.
Studies consistently show that finasteride’s long-term efficacy depends heavily on timing and individual response. The transplanted hair itself won’t fall out—it’s genetically resistant. What matters is protecting your remaining native hair.
| Timeline | Native Hair Retention | Transplant Survival | Key Finding |
|---|---|---|---|
| 5 years | 80-90% (with treatment) | 95%+ | Early use maximizes yield |
| 10 years | 70-85% (with treatment) | 95%+ | Consistent dosing matters |
| Untreated | 40-60% | 95%+ | Significant native loss |
The impact on yield isn’t about the transplant itself—it’s about preventing the need for future procedures. Without finasteride, you’re likely looking at ongoing miniaturization of existing hair, which complicates long-term aesthetics and may necessitate additional grafts down the line.
Making Your Decision: Questions to Ask Your Surgeon
The decision to start finasteride shouldn’t come down to what your surgeon recommends in isolation—it’s about understanding your specific hair loss pattern, your timeline for starting treatment, and whether the clinic’s post-operative protocol actually aligns with your goals.
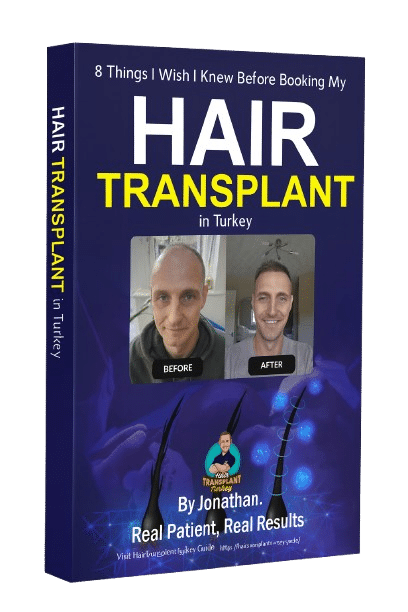
I learned this the hard way by asking too many general questions instead of the ones that mattered: How aggressive is my androgenetic alopecia likely to be? When should I realistically begin medication, and what happens if I wait? Does your surgeon’s aftercare plan include finasteride counseling, or are you expected to sort that out alone?
Your Personal Hair Loss Pattern
Before you commit to a hair transplant—whether in Turkey or elsewhere—you need to understand your own hair loss pattern, because it directly shapes what’s realistic for you to expect and how your surgeon will design your procedure.
Your genetics and patterns determine three critical things:
- How aggressively you’re losing hair — whether you’re in early-stage recession or advanced thinning affects graft placement and density goals.
- What underlying causes are at play — male pattern baldness behaves differently than diffuse thinning or post-surgical loss, and each requires different long-term strategies.
- Whether finasteride makes sense for you — if your loss is still active, medication protects non-transplanted hair; if you’re stable, your need changes.
Ask your surgeon to map your specific Norwood stage and predict your likely progression. That clarity matters more than any treatment decision.
Timeline For Starting Medication
The timing varies. Some surgeons recommend starting finasteride weeks before surgery to stabilize remaining hair.
Others suggest waiting until after initial healing—typically 2–4 weeks post-op—to avoid complicating recovery monitoring. A few prescribe it immediately after.
What matters most is consistency once you start. Finasteride requires continuous use to maintain results; stopping creates medication duration gaps that can reverse progress.
Ask your surgeon their specific protocol and *why* they recommend that timeline. The transplant timing shouldn’t dictate your decision—your hair loss pattern and overall health should.
Clinic’s Post-Operative Protocol
Because finasteride timing varies so widely between surgeons, you’ll want to understand exactly what your clinic recommends—and why.
When I consulted with my surgeon at Clinicana, they provided a clear post-operative protocol including specific medication guidance. Before you commit, ask your clinic:
- When should I start finasteride—immediately after surgery, or after a waiting period?
- Will they provide a prescription, or do I need to source it independently (noting potential off-label use considerations)?
- Do they monitor your response, and can you contact them if you experience side effects?
A reputable clinic should give you written aftercare instructions that include medication timing and dosage. This removes ambiguity and guarantees you’re following evidence-based protocol rather than guessing.
Frequently Asked Questions
Can I Start Finasteride Before Traveling to Turkey for My Transplant?
Yes, you can start finasteride before traveling. I’d recommend discussing timing with your clinic—they’ll want baseline before/after photographs and objective hair density evaluations to track your progress accurately throughout treatment.
Will Finasteride Affect the Transplant Procedure Itself or My Recovery Timeline?
No—finasteride won’t interfere with your transplant or recovery. I took it before surgery without complications. You’ll focus on post-surgery medication dosage with your clinic, then continue finasteride long-term for hair density maintenance.
If I Stop Finasteride, Will My Transplanted Hair Fall Out Like Native Hair?
No—transplanted hair won’t fall out if you stop finasteride. Those grafts are genetically resistant to DHT. However, your native hair will continue thinning, which is why finasteride dosage reduction requires careful consideration of your overall hair goals.
Does My Surgeon Need to Know I’m Already Taking Finasteride Before Surgery?
Yes, you absolutely need to tell your surgeon you’re already taking finasteride. I disclosed all my pre-existing medication details during my surgeon consultations—it’s essential for them to understand your full medical history and adjust your care plan accordingly.
How Do I Know if Finasteride Is Actually Working on My Remaining Hair?
You’ll notice finasteride’s working by tracking your hair shedding patterns over 6–12 months. If you’re losing less hair than before, experiencing slower recession, or seeing stable density, the medication’s effectively slowing loss. I’d photograph your hairline regularly for objective comparison.
Conclusion
You don’t need finasteride for your transplanted grafts to survive—they’re genetically resistant to DHT. However, I’d strongly recommend starting it around 3-4 months post-surgery to protect your native hair. You’ll likely retain 80-90% of your remaining hair at five years with consistent use. Discuss potential side effects with your surgeon before deciding, since your health matters more than perfect density.

 Continue with Google
Continue with Google