Hair transplants are generally very safe procedures – especially in expert hands – but it’s natural to be anxious about possible complications. You’ve probably seen horror stories on the internet: infections, “botched” results, or even people claiming their hair transplant failed. How common are these problems really? In this deep dive, we’ll separate fact from fear by examining the key hair transplant risks (infection, necrosis, shock loss, overharvesting, etc.) and how often they occur. We’ll also explore why the worst horror stories tend to come from certain ultra-low-cost clinics, and how choosing a hospital-based, regulated clinic can drastically reduce your risk. As someone who had a hair transplant in Turkey myself (and a very positive experience at a reputable Istanbul hospital clinic), I want to share both genuine expertise and firsthand perspective. By the end of this article, you’ll have a realistic understanding of hair transplant complications – and how to avoid becoming a horror story yourself.
Common Hair Transplant Complications and Their Incidence
Even the best surgeons will tell you: no surgery is 100% risk-free. Hair transplantation is no different, but it is a procedure with very low complication rates overall. Most side effects are minor and temporary (think swelling or scabbing). Serious complications are quite rare, and permanent damage is highly unusual when the procedure is done correctly. Let’s look at the most commonly discussed complications one by one – infection, necrosis, shock loss, and issues like overharvesting – and see how frequently they actually happen in modern hair restoration:
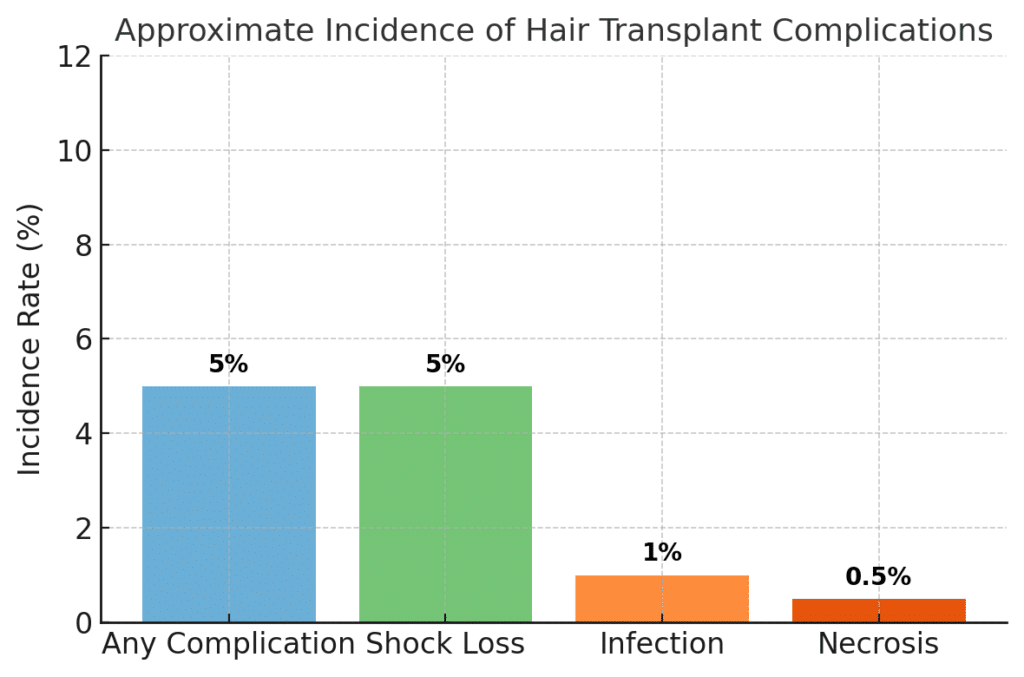
Chart: Approximate incidence rates of key hair transplant complications. Serious complications like infection or necrosis are well under 1% in proper clinical settings, while even temporary side effects (like “shock loss”) affect only a small minority of patients (linkedin.com). Overall, large studies show only around 1–5% of patients experience any significant complication at all.
Infection Risk
Infections are a top concern for any surgical patient. Fortunately, post-operative infection after a hair transplant is very uncommon. In clean, accredited clinics the infection rate is typically around 1% or less. For example, one published series of ~2,900 hair transplant patients reported only 2 cases of infection – that’s an incidence of about 0.07%. Those two patients had diabetes (a risk factor for poor healing), and their infections were mild and managed with basic treatment. Most surgeons will never encounter a severe deep infection in their hair transplant careers. (pmc.ncbi.nlm.nih.gov)
Why is infection so rare? Hair transplants involve small incisions and are done with tumescent local anesthesia (which has some antibacterial benefit). A reputable clinic strictly follows sterile protocols – surgical gloves, single-use instruments or proper autoclaving, antiseptic prep of the scalp, etc. – so the chance for bacteria to enter wounds is minimal. Preventive antibiotics are sometimes given as well. In my own surgery, for instance, I was in a full hospital operating theater with a sterile field; I went home with a short course of antibiotics as precaution, and I had no signs of infection at all.
It’s worth noting that minor surface infections can occur occasionally in the form of folliculitis – essentially a few small pimples or ingrown hairs as the grafts heal. This happens in a few percent of patients and is usually minor and easily treated (warm compresses or an antibiotic ointment). True serious infections (deep abscesses or systemic infection) are extremely uncommon in hair transplants.
Outlier cases: The only time we see high infection rates are in unhygienic environments or poorly managed cases. A broad 2025 review noted infection rates “up to 11%” in some reports, but this included older studies and perhaps less stringent settings. Such a high number is not the norm today – it’s an outlier. In a modern accredited clinic, you can expect 1% or lower risk of infection, provided you also follow your post-op care instructions (keeping the area clean, etc.). Essentially, if you choose a good clinic, infection should be the least of your worries. (linkedin.com)
Necrosis (Tissue Death)
Necrosis means localized tissue death due to loss of blood supply – in a transplant context, it refers to patches of skin on the scalp (either donor or recipient area) that die and form a scar. Understandably, this is one of the most dreaded complications because if a patch of scalp skin dies, the hair follicles in that patch are lost permanently and it leaves a bald scar spot. The good news is that necrosis is extremely rare: studies put the incidence well under 1% of cases. One large study of 533 procedures found necrosis in only about 0.8% – less than one in a hundred patients.
When necrosis does (very rarely) happen, what’s going on? Essentially, the skin’s blood circulation gets compromised. In hair transplants, this can occur if too many grafts are densely packed into a small area without enough blood supply, or from excessive use of epinephrine (adrenaline) causing prolonged vasoconstriction. It’s more likely in patients who are heavy smokers (smoking impairs circulation) or those with uncontrolled diabetes or vascular issues. Poor technique can also be a factor – for instance, an inexperienced technician implanting grafts with too much force or creating too much trauma could potentially damage the tissue. In recipient-area necrosis, the skin turns dark and scabby, and eventually an eschar (dead tissue) sloughs off leaving a depigmented scar spot. In donor-area necrosis, which is exceedingly rare, over-aggressive removal of grafts in one spot could theoretically starve that area of blood.
The key point is experienced surgeons know how to avoid necrosis. They limit graft density to safe levels, use vasoconstrictors sparingly, ensure the patient’s health is optimized (e.g. insisting on no smoking around the time of surgery), and handle tissues gently. In my case, my surgeon implanted at a high density but was careful to distribute grafts in a pattern that preserved blood flow. I also followed instructions not to smoke and to stay well-hydrated. The result: no necrosis, and pink healthy healing skin. For the vast majority of patients who go to skilled providers, necrosis is not something you will ever encounter. It’s a “worst-case” scenario that’s very unlikely when the transplant is done properly.
“Shock Loss” (Post-Op Shedding of Existing Hair)
Shock loss – also called effluvium – is a temporary shedding of your native hair after the surgery. Essentially, the “shock” of the transplant (from anesthesia, swelling, and surgical manipulation) can push surrounding hairs into a resting/shedding phase. A few weeks after the transplant, those existing hairs fall out suddenly, making the area look thinner before it gets better. This sounds scary, but shock loss is usually temporary – the hair grows back over the next 3–4 months in most cases. It’s a well-known phenomenon and not a true complication in the sense of damage, but it can be distressing if you aren’t warned to expect it.
Shock loss can happen in the recipient area (thinning of hairs that were originally in the transplanted zone, often those that were weak to begin with) and occasionally in the donor area around the extraction sites. How common is it? Reported rates vary: a 2025 review found recipient-site effluvium in up to ~6.5% of patients (about 1 in 15) and donor-area shedding in around 4%. Some other surgeons report lower numbers, especially in men. It tends to be more noticeable in women (who often have dense but diffuse thinning hair – shock loss of even some existing hairs can show since women are usually transplanting in between existing strands). In men, shock loss often affects miniaturized hairs that were on their last legs anyway. If those hairs shed, sometimes they don’t return (because male pattern baldness would have taken them soon regardless). But healthy hairs almost always come back after a resting phase. (linkedin.com)
Can we prevent or reduce it? Surgeons try to minimize trauma – using proper incision techniques and not excessively inflating the scalp with tumescent fluid – but some shock shedding is beyond control. One strategy is to use Minoxidil after surgery to speed up regrowth. Some doctors start minoxidil (Rogaine) a week or two post-op to stimulate follicles to re-enter growth phase faster, potentially shortening the shock loss period. In my own experience, I did notice some shedding of a few native hairs in the front about a month after surgery. It was mild, and by around month 4 I could see all the hair (transplanted + original) growing back and filling in. Essentially, shock loss was a non-issue long-term – but it was helpful that my clinic had counseled me beforehand that it might happen. When you know it’s normal, you won’t panic.
To sum up: shock loss can happen to a small percentage of patients, but it’s temporary and hair regrows in the vast majority of cases. It’s more of a temporary cosmetic inconvenience than a true complication. A year after your transplant, no one will be able to tell that those hairs shed – they’ll be back, along with your new transplanted hair.
Overharvesting & Permanent Donor Damage
One complication you might see in “horror story” photos is a visibly over-harvested donor area – patches of thinned-out hair or scarred spots on the back of the head where grafts were taken. Overharvesting means a clinic extracted too many follicles from the safe donor zone, or took them from the wrong areas, causing permanent damage or an unnaturally moth-eaten look. This is almost always the result of poor technique or greed, and it’s largely preventable by an ethical surgeon. Unlike infection or shock loss, overharvesting isn’t a random chance risk – it only happens if the clinic violates safe guidelines in an effort to yank out as many grafts as possible. Unfortunately, some bargain clinics do exactly that, leaving patients with a patchy donor region that may never fully recover.
Diagram: The “Safe Donor Area” (green) vs. unsafe zones (red) for graft extraction on the back of the scalp. Hairs in the safe zone are permanent and can be harvested in moderation without cosmetic thinning. Taking hair from outside this permanent band, or overharvesting too densely within it, risks permanent donor bald patches.
In a properly planned transplant, the surgeon will only harvest from the Safe Donor Area – the mid-back of scalp and sides above the ears where hair follicles are genetically resistant to balding. Even within this zone, there’s a limit to how many grafts can be safely taken. Typically, no more than about 15-20% of follicles in one area should be extracted in a single session; extractions should be spread out evenly so the remaining hair can cover any slight decrease in density. When clinics over-harvest, they might take 50% or more of the follicles from a spot, which the remaining hair can’t camouflage – resulting in visibly thin or bald patches in the donor. In extreme cases, entire patches of donor skin can even necrose if the trauma is too great and blood supply is compromised (this is rare, but cases have been reported when massive graft numbers were taken with large punches).
Overharvesting tends to happen in certain low-cost, high-volume clinics that promise absurd graft numbers or “mega sessions” without proper regard for the patient’s long-term donor management. The International Society of Hair Restoration Surgery (ISHRS) has warned that overharvesting and taking follicles outside the safe zone are among the greatest risks in unregulated clinics. The photo evidence can be heartbreaking: one ISHRS case showed a patient who “most likely went to a black market” clinic and ended up with an almost completely depleted donor area – an uncorrectable problem. Once those permanent follicles are over-harvested or scars replace them, you can’t magically get them back. (ishrs.org)
I want to emphasize that responsible clinics do not allow this to happen. My surgeon, for example, actually under-harvested a bit (leaving some grafts in reserve for the future) and made sure the extractions were uniformly distributed. Today, my donor looks essentially unchanged – no obvious patches or thickness difference. Ethical surgeons know that preserving the donor for the patient’s lifetime is crucial. They will often quote a slightly lower graft count and maintain a margin of safety, rather than gouge out every possible follicle. If a clinic is bragging about extremely high graft numbers or shows little regard for your donor appearance, that’s a huge red flag.
Bottom line: Overharvesting is a man-made complication – it’s a result of bad practice. Choose a reputable, experienced clinic and you shouldn’t have to worry about this at all. They will stay within safe donor limits. Unfortunately, many horror stories of patchy donor areas come from patients who went to cheap outfits that operated like a hair factory. We’ll talk more about those “hair mill” clinics next, and why they have higher rates of issues like this.
Why “Horror Story” Complications Cluster at Low-Cost Clinics
If hair transplant complications are generally so uncommon, why are there so many scary testimonials out there? The answer becomes clear when you look at where many of these botched hair transplant stories originate: a large number trace back to certain low-cost, high-volume clinic models. In places like Turkey (the world’s hair transplant hub), there are hundreds of clinics – and while many are excellent, some operate more like bargain assembly lines. These are sometimes referred to as “black market” clinics or hair mills, and they tend to be the source of most transplant horror stories. Let’s discuss what sets these operations apart and why their patients might experience higher complication rates.
High-volume, unlicensed operators: A defining feature of risky clinics is the lack of proper medical oversight. Often, technicians – who may have little or no formal medical training – perform most or all of the surgery, from harvesting grafts to making incisions. The actual doctor (if there even is one on site) might briefly draw the hairline and then disappear. The ISHRS has raised alarms about clinics where unlicensed techs (even “taxi drivers” in some extreme reports) are performing surgeries with minimal supervision. Such personnel are not qualified to handle surgical complications or make nuanced decisions, and they might not adhere to the strict hygiene standards that a board-certified surgeon would. This leads to increased risk of errors and infections. As Dr. Ricardo Mejia of the ISHRS described, patients at these clinics often don’t realize that an untrained person is doing the transplant until it’s too late.
“Factory” approach and corner-cutting: Low-cost hair mills make money on volume – they’ll schedule 5, 10, or even 15 patients in a single day. Naturally, this means each patient gets rushed attention. The focus is on speed, not finesse. Sloppy techniques (like using larger punches that can damage the donor or splitting grafts poorly) can creep in under such pressure. Sterilization might be compromised if multiple surgeries are happening simultaneously in the same room or if instruments aren’t properly re-sterilized between cases. As one hair restoration doctor put it, these outfits often cut corners to keep costs low – maybe reusing tools, or skipping the detailed patient prep and counseling that catches risk factors. The result? Higher complication rates. Indeed, an ISHRS member survey confirmed widespread patient harm from black-market clinics, including infections, scarring, graft wastage, and unnatural results.
Unrealistic graft numbers and overharvesting: We discussed overharvesting above – this is predominantly an issue at exactly these types of clinics. To entice customers, a shady clinic might promise “5000+ grafts in one session for $2000” – something a reputable surgeon would caution is too many for most patients. By trying to deliver that promise, they’ll overharvest the donor, using techs to pull as many grafts as possible. Patients have woken up to discover huge portions of their donor hair gone, yielding the kind of patchy bald spots that make the rounds on social media as cautionary tales. Similarly, these clinics might pack grafts too densely or implant into compromised scalp, leading to necrosis or poor growth. They often do not plan for the patient’s long-term hair loss progression – resulting in odd-looking implants that stand alone as surrounding native hair falls out over time.
Poor aesthetic design: Another “complication” (though not medical) is an unnatural hairline or bad overall cosmetic result. Many horror stories feature photos of pluggy, doll-like hairlines or grafts growing in the wrong direction. This usually happens when the personnel lack the artistry or training that experienced hair transplant surgeons have. Designing a hairline and angling each graft correctly is a skill that takes years to hone. In a black-market clinic, the tech placing your grafts might have been hired just last month. The ISHRS notes that unnatural hairlines and wrong graft direction are common problems reported from these outfits. Unfortunately, a botched aesthetic outcome can be just as devastating to a patient (requiring expensive repair work) as a medical complication.
No follow-up or recourse: Patients who encounter problems at sketchy clinics often find that aftercare is non-existent. Once you’ve paid and left, they may not respond to your concerns – especially if you traveled from abroad. There’s also little legal recourse; suing a clinic overseas for malpractice is usually impractical. This lack of accountability can embolden subpar providers. By contrast, reputable clinics invest in aftercare (regular follow-ups, detailed instructions, etc.) to ensure any issue is caught early and managed.
To put it bluntly, “you get what you pay for” in many cases. The reason some clinics can advertise transplant packages at a fraction of the cost is because they operate outside the proper standards. They rely on volume and often on unsuspecting international patients who are lured by the price. The horror stories we see – severe infections, grossly overharvested donors, terrible looking results – overwhelmingly come from these kinds of operations. The British Association of Hair Restoration Surgery and others have been calling for better regulation and patient education to combat this “black market” problem. As patients, the best thing we can do is avoid these clinics altogether. (https://www.itv.com/news/2025-08-20/it-was-horrific-uk-hair-transplant-patients-left-disfigured-and-scarred)
So how do you avoid them? The next section will cover exactly that: what a high-quality, hospital-based clinic does differently to virtually eliminate such risks, and how choosing the right provider is the ultimate safeguard for your hair transplant journey.
How Hospital-Based Clinics Minimize Risk and Ensure Success
If the nightmare scenarios are mostly tied to unregulated clinics, then the antidote is clear: choose a qualified, regulated clinic with an excellent medical reputation. In Turkey, some of the top hair transplant providers are those based in hospitals or specialized surgical centers that meet international health standards. From my own experience (having my transplant done at Clinicana within Acibadem Taksim Hospital in Istanbul), I can attest that a hospital-based clinic offers a level of safety and professionalism worlds apart from the bargain-basement shops. Here’s how these reputable clinics keep risks to an absolute minimum:
Flowchart: Comparison of a high-risk “hair mill” clinic model vs. a hospital-based clinic model. Reputable hospital clinics use licensed surgeons, strict medical protocols, and individualized care – leading to low complication rates and natural results. Black-market clinics often rely on unlicensed techs, cut corners on hygiene and technique, and push volume – leading to higher risks of infection, necrosis, poor growth, and other issues.
Professional medical staff: In a proper clinic, your surgery is physician-led. A certified hair transplant surgeon (often a dermatologist or plastic surgeon) designs and oversees the procedure. Crucially, Turkish law now mandates that the incisions and overall supervision be done by a doctor, not just technicians. At hospital clinics like mine, not only was the lead surgeon highly qualified, but the entire team of technicians were formally trained and experienced. This dramatically reduces the chance of human error. The difference is immediately noticeable – for instance, my surgeon spent a long time carefully drawing and adjusting my hairline and discussed the plan in detail, something fly-by-night places don’t do. As the ISHRS emphasizes, a physician-driven surgery (as opposed to technician-driven) is key to safety and success.
Certified, sterile facility: Being located in a hospital means the clinic adheres to hospital-grade sterilization and emergency protocols. The clinic I chose operates in a modern medical hospital under regulation by the Turkish Ministry of Health and ISO 9001 quality standards. This is not a random office with a bed; it’s a surgical unit with proper operating rooms, infection control, and all necessary equipment. All tools were either single-use or sterilized in an autoclave, and the staff followed surgical scrub procedures. These measures make the risk of infection incredibly low (close to zero in practice). If something like an allergic reaction or a rare complication were to occur, you’re literally in a hospital – full resuscitation equipment and specialists are right there. That peace of mind is huge. (Thankfully I didn’t need any of it, but it’s good to know it’s available!)
Reasonable case load and personalized care: Top clinics limit how many patients they do in a day. Often it’s one patient per day per team or a very low number, so that the focus is entirely on you. In my case, I was one of only one or two surgeries that day. The team was not rushing to finish; in fact, my procedure took nearly 7 hours with plenty of breaks to ensure everything was done meticulously. The atmosphere was calm and unrushed – they even had me come in the day before for blood tests and a heart check to be extra sure I was fit for surgery. This kind of thorough pre-op evaluation (and transparency about the process) is a hallmark of a good clinic. They screen out patients who aren’t good candidates and set realistic expectations, which prevents the “botched” outcomes born of bad planning.
Proper technique and technology: Hospital-based clinics tend to invest in the latest equipment and follow evidence-based best practices. For example, using fine punches and high-quality magnification to extract grafts causes less trauma to donor areas. Experienced surgeons also employ techniques to maximize graft survival – carefully handling grafts to avoid drying or damage, and storing them in optimal solutions. As a result, the graft survival rate in good clinics is extremely high (often 90–95% of transplanted grafts take and grow). This is why “failed hair transplants” are exceedingly rare at top clinics – nearly all the grafts will grow if transplanted correctly, leading to successful results for the patient. (For context, most modern hair transplants – done by experts – have over 90% success in terms of graft growth, which is why you see so many happy patients online!) If you see stats about low growth or transplants not working, it usually points back to poor technique at subpar clinics. (novahairtransplantnyc.com)
Safety protocols and backup: Reputable clinics have protocols to handle anything unexpected. They monitor your vitals during the procedure (I had a blood pressure cuff on, etc.), they have backup generators for power, they have emergency medications on hand. While hair surgery is under local anesthetic and very safe, these extra measures further reduce even one-in-a-million risks. Additionally, because they operate legally and under oversight, these clinics must maintain certain standards or they lose licensure. That external accountability (e.g. Ministry of Health inspections) keeps quality high.
Emphasis on aftercare: The duty of a good clinic doesn’t end when the surgery ends. I was given extensive post-op instructions, a kit with special shampoos, lotions, and medications, and a schedule for follow-up washes and check-ins. They actually brought me back the next day for a gentle hair wash and inspection of the grafts. This aftercare helps catch any early signs of trouble (like infection or excess swelling) and nip it in the bud. I also had direct WhatsApp access to the clinic’s medical team for months after – any question or concern I had was answered within minutes. Such support greatly reduces complications because if a patient does have an issue, the clinic addresses it promptly (e.g. prescribing antibiotics for a mild folliculitis before it could ever become an abscess). The British Association of Dermatologists stresses proper post-op care and hygiene as vital for good outcomes, and high-end clinics follow this philosophy closely.
Finally, regulation and credentials make a difference. My clinic proudly displayed its certifications, and I was comforted knowing the World Health Organization’s advice for medical tourists: choose providers that meet international safety standards – “Clinicana checked every box,” I remember noting. When a clinic is accredited and full of glowing real patient reviews (not just flashy marketing), you can bet they have a track record of low complications and satisfied patients.
In short, a hospital-based or well-regulated clinic virtually engineers out most of the risks. By having the right people, processes, and environment, they ensure that the already-low probability of complications drops even further. It’s no surprise that my outcome – and the outcomes of thousands who go to such clinics – have been overwhelmingly positive with no major complications at all.
Conclusion: Realistic Risks, Realistic Trust
A hair transplant can truly be life-changing – it certainly was for me – but it’s important to approach it with informed realism. The reality is that serious complications are exceedingly uncommon when you entrust your head to qualified experts. Infection, necrosis, severe scarring – these worst-case scenarios make headlines precisely because they’re rare, and they usually involve egregious lapses in proper technique or ethics. By sticking with reputable clinics, your odds of encountering a major complication are extremely low (on the order of less than a few percent overall). In contrast, your odds of getting a great result with restored hair are very high – most modern hair transplants have 90%+ success rates in terms of graft survival and patient satisfaction.
That said, “low risk” doesn’t mean “no risk.” Any surgery has some degree of chance for unexpected issues. You might be that 1 in 300 or 1 in 1000 who gets an infection or some grafts that don’t grow as well. It’s important to be aware of these possibilities without letting fear paralyze you. From my journey, I can say that being informed actually increased my confidence – I knew what warning signs to watch for and I chose a clinic that had plans in place for every scenario. This knowledge is empowering.
If you’re considering a hair transplant in Turkey (or anywhere), do your homework on the clinic. Insist on seeing the surgeon’s credentials, ask about their complication rates, look for independent patient reviews. A trustworthy clinic will be transparent and will prioritize your safety over sales. Remember, the clinics with thousands of happy clients and tons of 5-star reviews achieve those results by consistently avoiding complications – that doesn’t happen by accident, but through high standards.
Lastly, as a patient, you play a role in your own success too. Follow the pre- and post-op instructions your clinic gives. Many complications (like infection or poor growth) can be mitigated by proper self-care: keeping the area clean, avoiding smoking, taking your meds, and going to follow-ups. I was almost obsessive about my post-op care (because hey, I wanted the best outcome!), and it paid off in a smooth recovery.
To recap the key takeaways:
- Hair transplant complications are real but rare – most people won’t experience anything beyond transient discomfort, provided they choose a good clinic.
- The main potential issues (infection, necrosis, shock loss, overharvesting) have incidence rates typically below 1–5%, and nearly all are preventable or manageable when experts are in charge.
- Horror stories tend to come from cut-rate clinics that ignore these safeguards. Avoiding such clinics hugely tilts the odds in your favor.
- A hospital-based, regulated clinic with an experienced surgeon offers the safest environment – essentially replicating the conditions that keep complication rates near zero.
- My personal experience is testament: I encountered no serious complications whatsoever. By 7 months post-op, I have a full, natural hairline and a healthy donor area – and no one would ever guess I had surgery, which is the ultimate sign of a successful, well-done transplant.
In the end, the goal of discussing complications is not to scare, but to educate and build trust. Knowing the real numbers and causes helps you make wise decisions. I hope this deep dive has given you a reassuring sense of medical realism: hair transplants are not wild gambles with your appearance or health – they are, in fact, one of the safest cosmetic surgeries when done right. With the right clinic and proper care, the only “complication” you’re likely to face is explaining to your friends how you suddenly grew all that hair!
Stay informed, choose wisely, and you can look forward to joining the thousands of us enjoying our results – with no horror story to tell, only a success story. Here’s to a safe and satisfying hair transplant journey.
Sources: High-authority references and medical studies were used to support the facts in this article, including peer-reviewed research on complication rates, ISHRS guidelines on safe practices, and reputable medical resources on hair transplant success rates. These ensure that the information provided reflects the latest understanding and statistics in the field of hair restoration surgery.

 Continue with Google
Continue with Google