A deep dive into success rates, graft survival, and why some transplants fail
As someone who underwent a hair transplant in Turkey, I know firsthand that a “successful” result means more than just a big graft number on paper. After my procedure, I dove into research from medical journals and organizations like ISHRS to understand why some transplants thrive and others fail. In this guide, I’ll share that deep research and personal insight – from defining what true success looks like (graft survival, density, aesthetics, and satisfaction) to comparing FUE vs. DHI techniques, the importance of a surgeon-led approach, the truth behind mega-sessions of 5000+ grafts, common failure causes, and even a timeline of hair growth after surgery.
My goal is to help you set realistic expectations and avoid the mistakes I learned to dodge.
What Does “Success” Mean in a Hair Transplant?
When we talk about a successful hair transplant, we’re really talking about a combination of factors coming together to meet the patient’s goals:
- High graft survival rate: This is the percentage of transplanted grafts that ultimately take root and grow hair. In modern clinics with skilled surgeons, over 90% of grafts usually survive and grow in the new area (turkeyhaircenter.com). In fact, when a hair transplant is done correctly under optimal conditions, studies show 76–95% of grafts successfully grow, especially in healthy, non-smoking patients (envoyhealth.io). A high survival rate means you truly get the hair you paid for.
- Adequate density: Density is measured in grafts per square centimeter (grafts/cm²). A natural-looking result doesn’t require restoring the original juvenile density (which might be 80–100 follicular units per cm² on a full head of hair). In practice, transplanting 35–50 grafts per cm² can create the appearance of full hair coverage (forhair.comforhair.com). Top surgeons often target around 40 grafts/cm² in most areas – this achieves a thick look while still being safe for graft survival. Cramming grafts too densely can actually backfire; if you try to “dense pack” far beyond 50–60 grafts/cm², the scalp’s blood supply can’t nourish all grafts, and survival drops. (One clinical analysis found nearly 100% survival at 30 grafts/cm², but only ~84% survival at 50 grafts/cm² due to congestion and healing issues (forhair.com).) Success is about finding the sweet spot – enough grafts to look full, but not so many that they die off or scar your scalp.
- Artful aesthetics: I learned that technical success means nothing if the result doesn’t look natural. A successful transplant should have an age-appropriate, natural hairline design and proper graft placement. This includes careful attention to hair angulation, direction, and randomization so that the transplanted hair mimics how real hair grows. For example, single-hair grafts are used at the hairline to create a soft, feathered look, with denser follicular units placed behind for volume. In my case, the surgeon spent a good hour just designing the hairline and temple angles. Aesthetic success means no “pluggy” look, no odd tufted areas – just hair that suits your face as if nature gave it. It’s hard to put a number on aesthetics, but patient satisfaction is a good proxy. If it looks natural and dense, you’ll feel it was a success. Surveys show that when transplants are done well, patient satisfaction rates often exceed 90% (turkeyhaircenter.com) – meaning the vast majority of patients are happy with how their hair looks.
- Patient satisfaction and confidence: Ultimately, the true measure of success is your satisfaction. Did the procedure meet your goals and improve your quality of life? This is subjective, but absolutely vital. A transplant could have high graft survival and density, but if the hairline shape or overall look isn’t what the patient hoped for, they may feel it wasn’t “successful.” On the other hand, even a smaller procedure that restores a natural frame to the face can be life-changing for a patient’s confidence. In my experience, waking up and seeing a hairline instead of a bald forehead in the mirror was the moment I knew my transplant was a success. Medical literature echoes this: a successful hair restoration is one that achieves patient satisfaction in terms of cosmetic improvement and self-esteem, not just surgical metrics.
In short, “success” in hair transplantation is multi-factorial – it means the grafts survived, the hair grew with good density, the result looks natural, and the patient feels it was worth it. Keeping all these elements in mind will help you evaluate clinics and set the right expectations for your outcome.
FUE vs. DHI: Survival Rate Statistics and Outcomes
Follicular Unit Extraction (FUE) and Direct Hair Implantation (DHI) are two popular techniques in Turkey and worldwide. A big question I had was: does one method produce a higher graft survival rate or better results than the other? I dug into the research to separate marketing claims from reality.
Figure: A comparison of average graft survival rates after 12 months for FUE and DHI techniques. Studies show both methods yield very high survival (around 90–95%) when performed properly (turkeyhaircenter.com). In a 2024 clinical study, FUE grafts had about a 91% survival rate vs. 93% for DHI – a difference so small it wasn’t statistically significant (turkeyhaircenter.com).
What the evidence says: According to the International Society of Hair Restoration Surgery (ISHRS), the average graft survival rate is 85–95% for both FUE and DHI under sterile technique with a skilled team (turkeyhaircenter.com). In other words, both techniques are capable of excellent outcomes. A recent published analysis of 160 patients in the Journal of Cosmetic Dermatology (2024) found FUE grafts had a 91.4% survival rate vs. 93.2% for DHI after one year – essentially equal success when done by experienced surgeons (turkeyhaircenter.com). My own transplant was FUE and I was quoted a ~95% expected survival, which aligns with these figures.
Why DHI is sometimes marketed as superior: You’ll see some clinics (especially those specializing in DHI) claim that DHI has a higher survival rate – often citing numbers like 97–98% graft survival (drserkanaygin.com). The rationale is that with DHI, grafts are implanted immediately using an implanter pen (Choi pen) without needing to first create recipient incisions. This direct implantation keeps grafts out of the body for a very short time, theoretically reducing dehydration or damage to the follicles. In fact, the DHI technique was designed to minimize the “time out of body” for grafts to maximize survival (pmc.ncbi.nlm.nih.gov). In contrast, standard FUE involves extracting grafts first, holding them in a solution (often chilled saline) while hundreds or thousands are collected, then making incisions, then implanting. That process can mean grafts spend an hour or more outside the body. One in vivo study by Limmer on graft storage found about 1% loss of viability per hour of grafts being out of the body (e.g. ~95% survival at 2 hours vs ~90% at 4 hours) (pmc.ncbi.nlm.nih.gov). DHI aims to eliminate this issue by inserting grafts within minutes of extraction. So on paper, DHI could yield slightly higher survival due to less drying or trauma to grafts.
What happens in practice: If the surgery is well-executed, both FUE and DHI have outstanding survival rates (usually 90%+). The slight theoretical edge of DHI doesn’t automatically guarantee a better result in the real world, because a lot depends on the surgical team’s skill and how grafts are handled. A high-volume FUE clinic in Turkey that uses proper graft hydration and quick implantation can achieve equal survival to a DHI procedure. In fact, many surgeons will tell you that the surgeon’s technique and graft handling matter far more than the choice of FUE vs. DHI (turkeyhaircenter.com). My research bore this out: one hair restoration doctor put it this way – “The method is only as good as the hands performing it.” (turkeyhaircenter.com). An expert FUE surgeon who minimizes graft trauma can get 95%+ growth, while a poorly done DHI by untrained techs could fail to hit those marks.
Bottom line on FUE vs DHI outcomes: Both FUE and DHI, when done by qualified surgeons, yield permanent results and high growth rates. They mainly differ in how grafts are implanted, which can affect other aspects like speed, cost, and the number of grafts done in a session (more on that later). For survival rates, peer-reviewed studies find no significant difference if all else is equal (turkeyhaircenter.com). I chose FUE for my transplant due to the larger area I needed to cover, and my results (around 12 months later I have thick, natural hair growth) are on par with friends of mine who chose DHI. If you are leaning toward DHI because you’ve heard it’s “more effective,” keep in mind it’s not a magic bullet – the expertise of the clinic is still the deciding factor. The main benefit of DHI is precision in implanting (which can be great for creating natural hairlines or doing smaller touch-ups) and slightly faster recovery of the recipient area. The main drawback is DHI is slower and usually more expensive, since implanting with a Choi pen is labor-intensive (often limited to ~2,500 grafts per session vs. 3,000–4,000+ grafts in a day with FUE) (turkeyhaircenter.comturkeyhaircenter.com).
In summary, expect over 90% of grafts to grow whether you choose FUE or DHI – provided you choose a reputable, experienced team. Don’t be swayed by glossy marketing that touts nearly 100% success; in reality both techniques are extremely effective, and the small differences in graft survivability will come down to surgical finesse, not the hype around a particular tool.

Surgeon-Led vs. Technician-Led Clinics: Why It Matters
One of the most crucial factors for hair transplant success – and one often overlooked by eager patients – is who is actually performing the surgery and how involved the surgeon is throughout the process. In Turkey, you’ll encounter both surgeon-led clinics and more commercial technician-led operations. Having experienced a clinic where the surgeon was hands-on, and hearing horror stories from those who weren’t so lucky, I can’t stress enough: the skill and oversight of a qualified surgeon directly affect graft survival, aesthetic outcome, and the risk of complications or failure.
Here’s what the research and my experience show:
- Surgical expertise vs. assembly line clinics: The ISHRS has issued consumer alerts about so-called “black market” hair clinics abroad that lure patients with low prices, only for the surgery to be mostly done by unlicensed technicians with minimal supervision (ishrs.orgishrs.org). In these cases, the results can be disastrous. Common problems reported from technician-run surgeries include severe scarring, unnatural hairlines, poor hair growth, hairs growing in the wrong direction, and over-harvested donor areas that leave bald patches (ishrs.org). In fact, members of ISHRS noted that some patients were promised 4,000–6,000 grafts by such clinics “assembly line” style, but later discovered they only received half that number – essentially being cheated on graft count (ishrs.org). The take-home point: if the doctor isn’t closely involved, your risk of a botched outcome shoots up. I deliberately chose a clinic known for having the surgeon perform the critical steps (designing the hairline, doing the graft extractions, and making the recipient incisions) with a well-trained team assisting, because I wanted those expert eyes on my grafts.
- Surgeon involvement improves survival and aesthetics: A skilled surgeon brings both technical know-how and an artistic eye. From a survival standpoint, an experienced surgeon will implement protocols to maximize graft viability – things like using the proper punch size to avoid transecting follicles, carefully handling grafts by the bulb, keeping them moist and chilled, and limiting time out of the body. Research by Bernstein et al. emphasizes continuous supervision of the staff throughout the procedure to ensure optimal graft handling, because grafts are fragile from the moment they leave the scalp until about a week after implantation (pmc.ncbi.nlm.nih.gov). In delicate microsurgery like this, an untrained tech might crush a graft with forceps or let it dry out in the pan, but a veteran surgeon (or a tech under their close guidance) will avoid those mistakes. (Some of the biggest graft killers are mechanical trauma, desiccation, prolonged hypoxia, or improper storage solution (pmc.ncbi.nlm.nih.gov) – all of which are preventable with proper technique.) On the aesthetic side, a surgeon will know how to create a natural hairline that suits your face and age, whereas a non-expert might place grafts in straight rows or at wrong angles, yielding a pluggy look. For example, DHI implantation requires millimeter-perfect control of angle, depth, and direction; if that task is delegated to unlicensed techs, “the results will often look pluggy or unnatural,” warns Dr. Serkan Aygın, a top hair surgeon (drserkanaygin.com). Many top Turkish clinics actually limit the role of technicians to assisting tasks like graft counting and sorting, while the surgeon does or oversees the rest – this model tends to produce the best outcomes.
- The dangers of technician-run surgeries: Without proper medical training, technicians may also mismanage the donor harvesting – taking too many grafts from one area or outside the safe donor zone. I’ve seen cases where a patient’s donor area was left looking moth-eaten and scarred because an unsupervised tech over-harvested in the rush to hit a high graft number. The ISHRS warns that these practices can deplete the donor permanently and leave obvious bald spots in back of the head (ishrs.org). Unqualified personnel might also skip important steps like proper sterilization or patient evaluation, leading to infections or graft necrosis. And if something goes wrong (say, excessive bleeding or a bad drug reaction), an unlicensed provider will not know how to respond – a very scary thought. There’s also virtually no legal recourse if a non-doctor messes up your surgery in a foreign country (ishrs.org). This is why ISHRS urges patients: verify who will actually be doing the transplant. If it’s not a licensed, experienced physician (or at least under the immediate supervision of one), walk away (ishrs.org). Your results and safety are at stake.
- “Team” approach done right: This is not to say technicians have no place – hair restoration is often a team effort. In a proper clinic, a team of medical technicians might assist by trimming grafts or placing them into pre-made sites under the surgeon’s direction. Many excellent surgeons train their technicians extensively. The key is that the surgeon is in control and accountable for the surgery from start to finish. For instance, in my transplant, the surgeon did all the FUE extractions and made the recipient incisions. Two techs then implanted the grafts into those sites. However, the surgeon was right there the entire time, periodically checking placement, and the most difficult grafts or hairline implants he did personally. This ensured consistency and care. In one published technique (Direct Hair Transplantation, a modification of FUE), the authors noted that by having the physician implant the most difficult grafts and continuously oversee the process, the whole operation was better streamlined to ensure graft survival (pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov). They even coined the term “H-factor” (human factor) for poor results caused by human error – e.g. improper graft handling or staff fatigue – underscoring that vigilant oversight is needed to avoid these pitfalls (pmc.ncbi.nlm.nih.gov).
In summary, a surgeon-led clinic with a qualified team will generally yield higher survival rates, a better-looking result, and fewer complications than a technician-driven “hair mill.” As a patient, doing your homework on who will be performing your surgery is critical. Don’t be afraid to ask clinics directly: Will the certified surgeon be harvesting my grafts and designing the sites? How experienced are the staff who assist? In my case, choosing a slightly more expensive clinic that prioritized physician involvement paid off – I have a natural hairline and strong growth. The extra peace of mind was worth it, knowing I wasn’t in the hands of, as ISHRS put it, a possible “taxi cab driver” turned hair tech operating on an assembly line (ishrs.org). It might sound extreme, but those places exist. Stack the odds in your favor by opting for medical expertise over rock-bottom price.
The “5000 Grafts” Hype – Mega Sessions vs. Realistic Planning
If you browse hair transplant ads, especially from some clinics in Turkey, you’ll inevitably see boasts like “We transplant 5,000+ grafts in one session!” On the surface, it sounds amazing – more grafts = more hair, right? I certainly was tempted by the idea that a single mega-session could cure my baldness. However, through both research and candid talks with my surgeon, I learned that chasing huge graft numbers in one surgery can be misleading at best and dangerous at worst. Here’s why those ultra-high graft promises often don’t equal success:
- Donor area limitations: Every patient has a finite supply of “permanent” donor hair at the back/sides of the scalp. On average, the safe donor zone contains around 6,000–7,000 grafts total that could ever be harvested over multiple procedures (advancedhair.com). Extracting 5,000+ grafts in one go means you’re draining a huge portion of your reserves in a single session. For some patients with exceptional density, this might be technically possible, but for many it would require overharvesting – either taking too many follicles from one spot (causing visible thinning or patchy scars) or extending outside the true safe zone (taking hair that isn’t actually permanent). An ethical surgeon will aim to harvest no more than about 30%–35% of the follicles in any given donor area (advancedhair.comadvancedhair.com). That usually translates to maybe 2,000–4,000 grafts in one surgery for most people. When you see clinics pushing 5,000–6,000 grafts, beware: they might be exceeding safe limits. Overharvesting can lead to a moth-eaten donor appearance, or worse, loss of native hair around the extraction sites. Some unscrupulous clinics even harvest from the nape or upper sides (outside the safe zone) to boost graft counts – but those hairs often thin out over time due to androgenetic alopecia, meaning the transplanted hair could fall out after a few years, defeating the purpose (advancedhair.com). Realistic promises respect the donor area’s long-term integrity.
- Surgery duration and graft quality: Let’s say a clinic truly attempts a 5,000 graft FUE mega-session. Consider that extracting that many grafts usually takes many hours (often 6–10+ hours of operating). Prolonged surgery times increase risks for both the patient and the grafts. A procedure stretching 8 or 9 hours means the latter grafts are sitting out for a very long time before implantation, which can reduce their survival (recall the ~1% per hour loss rule) (pmc.ncbi.nlm.nih.gov). It also means the medical team may become fatigued, increasing the chance of errors like transecting follicles or placing grafts sloppily. From the patient side, longer anesthesia and operative time raise the risk of complications such as bleeding, hypotension, or infection. Indeed, doctors do not usually recommend transplanting 5,000+ follicles in one session because of these issues: one session that long can result in “diminishing returns” on graft survival and more post-op discomfort (healnhub.comhealnhub.com). One medical article noted that a 5,000-graft transplant could take 7–9 hours, and the prolonged operative stress increases risks of infection, prolonged anesthesia effects, and graft drying or mishandling toward the end (healnhub.com). I was in the chair for about 7 hours for ~3,500 grafts and honestly I was exhausted by the end – I can’t imagine pushing that much longer and expecting top-quality work throughout.
- Overharvesting and donor damage: We touched on this, but to emphasize: taking too many grafts at once can permanently damage your donor area. Overzealous extraction can lead to visible empty spots or diffuse thinning in the back of your head. It can also cause scarring that makes further transplants difficult. Clinics that brag about huge sessions sometimes prioritize the immediate cosmetic goal (max grafts) over the long-term health of your donor. As one hair restoration practice explains, “Your donor hair is a precious, limited resource… Overharvesting – taking too many grafts from any one area – can be detrimental to your overall result” (advancedhair.comadvancedhair.com). A responsible surgeon will spread out extractions and may suggest multiple surgeries if you truly need 5000+ grafts, instead of doing it all at once (healnhub.com). In many cases, dividing into two sessions on separate days (or visits) yields better overall growth and allows the donor to heal in between. When I discussed graft count with my clinic, they actually refused to go for an overly ambitious number in one day – and I’m glad they set that boundary for my safety.
- Unrealistic marketing and graft count inflation: It’s worth noting that some clinics play fast and loose with graft numbers in their ads. The ISHRS has highlighted cases where patients were told, for example, that 5,000 grafts were implanted, when in reality maybe 2,500 grafts were (the clinic doubled the number by counting hairs or simply lying) (ishrs.org). Since most patients can’t verify the count themselves, this kind of false advertising happens. So, a claim of “5000 grafts” might not even be true. And if it is, it might include weaker two-hair grafts split into singles or other tricks to pad the stats. My advice: be cautious of too-good-to-be-true numbers. Focus on the quality of grafts and strategic placement rather than just quantity.
- Balancing coverage vs. density vs. safety: Some patients with very advanced baldness (Norwood 6–7) may indeed need around 5,000 grafts to achieve their desired coverage over multiple areas. But even in those cases, many top surgeons prefer a combined approach (FUE + FUT) or two-stage FUE to safely move that many grafts. Combining FUT (strip surgery) with FUE can yield 5,000+ grafts in one visit from two methods, which can be safer on the donor than 5,000 FUE extractions alone. The key is proper planning: mapping out which areas to cover now and which to address later, to avoid overharvesting or creating a sparsely covered result. There’s also the concept of diminishing aesthetic returns – past a certain number, adding more grafts in one surgery yields very little visible improvement but greatly increases risk. Often, “less is more” in hair transplantation. A modest, well-done 3,000 graft transplant can look better than a rushed 5,000 graft job that results in shock loss or poor growth.
To illustrate, why don’t doctors recommend trying to plant 5,000+ grafts in one go? Medical consensus points to these reasons: (1) Surgery longer than 6–7 hours raises complication risk (infection, anesthesia issues) (healnhub.com). (2) Extracting that many grafts can traumatize the donor area – causing scars or thinning from overharvesting (healnhub.com). (3) Grafts implanted after hour 8 or 9 might not get optimal care, leading to placement errors (wrong angle/depth) or drying out, which means lower yield (healnhub.com). (4) The patient’s head can only handle so much scarring at once; creating too many recipient sites densely packed can risk blood supply issues (grafts competing for nutrients). (5) Recovery from an ultra-mega-session is tougher – more swelling, longer healing, more intense post-op shedding.
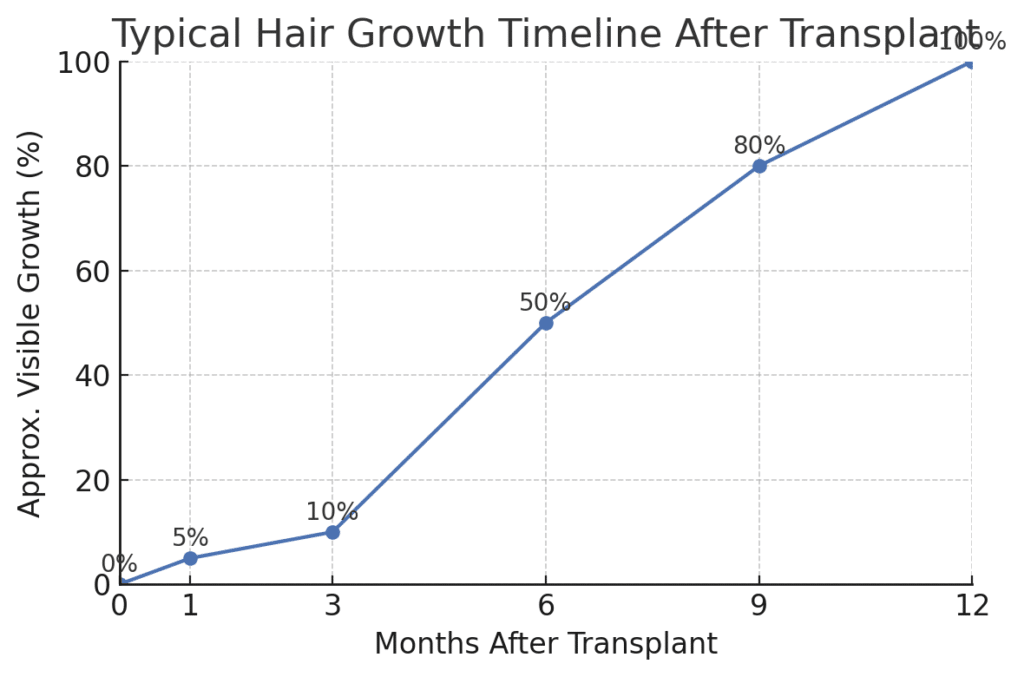
Figure: Typical hair growth timeline following a transplant (illustrative). Transplanted hairs often shedding in the first 2–4 weeks, then start to regrow over the ensuing months. By ~6 months post-op, about 50% of the final hair growth is usually visible (forhair.com). Results continue improving, with full growth maturing around 12–15 months after surgery (newsnetwork.mayoclinic.org). (Individual timelines vary – some patients see new growth as early as 3 months, others closer to 5 months. Patience is key!)
The safer strategy promoted by many surgeons (and what I personally did) is to split large graft needs into multiple surgeries. I had roughly 3,500 grafts and even that was done over two consecutive days. Some clinics might do 3,000 one day and 2,000 the next for a total of 5k in one trip, which can be okay because each day’s work stays in the safe zone for graft survival. If you truly require a second transplant for more density or coverage, plan it after you’ve seen the results of the first (usually at least 6–12 months later). This staged approach ensures you don’t run out of donor hair and allows the surgeon to refine the plan based on how you responded to the first transplant.
In conclusion, be wary of the “one-session mega transplant” sales pitch. Quality and careful planning trump sheer quantity. Unrealistic high graft counts in one session may lead to failure risks, overharvesting damage, or subpar growth. A reputable clinic will design a master plan for you – which may involve a sensible number of grafts in one sitting and possibly a second round down the line. Remember, a successful outcome is about how the end result looks, not whether you can brag about getting 5,000 grafts in a day. Often, less is more when done with artistry and care.
Common Causes of Hair Transplant Failure (and How to Avoid Them)
While modern hair transplants have a high overall success rate, not every surgery yields a happy patient. As I researched what could have gone wrong, I identified several common causes of hair transplant failure. Knowing these can help you steer clear of subpar clinics and practices:
- Poor surgical planning: A flawed game plan leads to flawed results. This can mean designing an inappropriate hairline (too low, too straight, or not accounting for future hair loss progression), mis-estimating the number of grafts needed, or distributing grafts poorly. For example, if a young patient’s transplant covers his front but he keeps losing hair behind it, he’ll end up with an “island” of transplanted hair – an unnatural look. Proper planning involves measuring donor density, projecting future loss, and prioritizing areas that yield the most cosmetic benefit. A failure in planning can also be using the wrong technique for the case (e.g. attempting DHI on a very large bald area which is inefficient, or doing only FUE when the patient’s donor characteristics may have supported a FUT strip for more grafts). Essentially, one size does not fit all – and an inexperienced surgeon might not customize the plan appropriately. During my consultation, the doctor carefully examined my donor reserves and even turned me away initially because my hair loss wasn’t “mature” enough (I was advised to treat medically first). That kind of honest planning helps avoid an “oops” transplant that fails a few years later.
- “Overharvesting” the donor: This is a subset of poor planning but deserves emphasis. As discussed earlier, taking too many grafts from the donor area can cause visible thinning or scarring in the back of the scalp – a telltale sign of a transplant gone wrong. Not only does this look bad, it also reduces the pool of grafts available for any future touch-ups or procedures (advancedhair.com). If a clinic depletes your donor in one go and you’re not satisfied with the result, you may not have a second chance. Signs of overharvesting to watch for post-op include wide gaps between extraction sites, a moth-eaten appearance, or the donor scalp feeling unstable. Avoid this by going to a clinic that values donor management – they should only take a safe percentage and do so evenly across the donor zone. The ISHRS even launched a campaign against such unethical practices because many patients have been scarred by clinics that “chased graft counts” and ruined their donor area (advancedhair.com).
- Unqualified or unsanitary clinics: This ties into the surgeon vs. tech discussion. A common cause of failures is simply choosing a bad clinic – one that maybe spends more on Instagram ads than on quality control. Indicators include lack of proper medical licensing, unclear who the surgeon is, very low prices that seem too good, or high-pressure sales tactics. These clinics might use cheap instruments, reuse punches or implanters without proper sterilization, or operate almost like a factory. The outcomes can be disastrous: infections, grafts placed poorly, hair growing in strange directions, or massive shedding due to trauma. The ISHRS warns that many patients lured to such outfits end up with botched results like scarred scalps and disfigured hairlines (ishrs.org). If an infection occurs (from non-sterile technique), grafts can die en masse – an obvious failure. Always verify the clinic’s credentials, read reviews, and ensure they follow rigorous hygiene protocols. In my journey, I skipped any clinic that didn’t let me speak to the actual surgeon or evaded questions about who performs what. Trust your gut – if it looks shady, it probably is.
- Improper graft handling and placement: Even in a decent clinic, things can go wrong if the team is careless. Each follicular unit is tiny and delicate. If grafts are crushed, pinched, dried out, or forced into incisions with too much pressure, their survival rate plummets. This can lead to a poor yield (patchy growth or many grafts that never produce hair). Proper technique requires delicately holding grafts by the edges, keeping them moist in chilled saline or PRP, and placing them into sites that are the right size. If sites are too tight or the angle is off, grafts can be damaged or “popped” back out. I’ve heard of cases where inexperienced staff implanted grafts at the wrong angle, resulting in hairs that stick out or lay flat incorrectly – essentially a failed aesthetic result that might require correction. This is why an attentive surgeon supervising (or performing) the implantation phase is crucial. Continuous irrigation of grafts, using magnification to handle them, and limiting time out of the body are all best practices to avoid this cause of failure (pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov).
- Lack of postoperative care (by the patient or clinic): Believe it or not, what happens after the surgery can make or break the success of a hair transplant. The first 7–10 days are critical for graft survival – the follicles are trying to secure blood supply in their new location. If a patient neglects the post-op instructions, they can lose grafts before they ever grow. For instance, knocking the grafts (bumping your head, vigorous rubbing while washing) in the first few days can dislodge them. In fact, grafts are only firmly “anchored” after around 8–10 days (pmc.ncbi.nlm.nih.gov), so you have to baby them initially. Not following the cleaning protocol can lead to crust build-up, which might make grafts fall out when the scabs come off. Likewise, poor hygiene or early exposure of the scalp to dirt and sweat can invite infection, which can kill grafts or cause scarring. Clinics should provide detailed aftercare guidance – and good ones include multiple follow-up washes and check-ups. (My clinic had me come in the next day for a gentle wash and provided an aftercare kit with saline spray, special shampoo, etc.) If a clinic doesn’t emphasize aftercare, that’s a red flag. And as a patient, you must take it seriously: avoid smoking (which impairs blood flow to grafts), don’t scratch or pick at scabs, sleep with your head elevated, avoid strenuous exercise for a couple of weeks, and keep the scalp clean and moisturized as instructed. One aftercare article put it well: neglecting post-op care can result in shedding, weaker growth, and graft failure – while diligent care gives your grafts the best chance to “take” and thrive (gracetouchclinic.com). In short, you have a role in your transplant’s success. Think of the grafts like seeds; the surgeon plants them, but you must water and protect them in the early days. Even with perfect surgery, ignoring aftercare can ruin the outcome.
- Patient factors and unrealistic expectations: Lastly, failure can sometimes be in the eye of the beholder. A transplant might actually yield decent growth, but if the patient expected a miracle (like teenage-level density on a totally bald head), they’ll be disappointed. Setting realistic expectations is key to feeling that your transplant succeeded. Additionally, certain patient factors (smoking, underlying health issues like uncontrolled diabetes, or severe scar tissue in the scalp) can reduce success rates. Some forms of hair loss (like aggressive alopecia areata or active lichen planopilaris) are prone to poor outcomes – these should be screened out by the doctor beforehand. A good clinic will educate and select patients properly to avoid doing transplants on unsuitable candidates. If those steps are skipped, the risk of “failure” (either medically or in the patient’s mind) rises.
How to avoid these failure modes? Choose your clinic and surgeon with care, plan the surgery conservatively with future needs in mind, follow all aftercare instructions, and keep expectations grounded. I found that doing my homework – reading medical publications and patient forums – helped me differentiate quality providers from flashy pretenders. The result is that I avoided the major pitfalls and ended up with a successful outcome I’m thrilled with. If you cover the bases we’ve discussed, you can dramatically tilt the odds of success in your favor.
Conclusion
A hair transplant can truly be a life-changing procedure – I can attest to the boost in confidence and happiness seeing my new hair grow in. But achieving great survival rates & outcomes isn’t a matter of luck; it comes from informed decisions and high standards at every step of the process. We defined success beyond just graft counts, looking at the importance of graft viability, density, and natural aesthetics (ultimately measured by your satisfaction). We saw that FUE and DHI methods both deliver excellent survival (90%+) when done by experts (turkeyhaircenter.com), with no method having a monopoly on success despite what marketing might claim. We highlighted how surgeon-led care trumps technician-run mills – having a skilled, ethical surgeon at the helm makes all the difference in avoiding scars, ugly hairlines, or graft wastage (ishrs.orgdrserkanaygin.com). We debunked the “5000 grafts in one session” sales gimmick by explaining the real risks of mega-sessions – from overharvesting your donor to diminishing graft quality (healnhub.comadvancedhair.com). And we broke down the common causes of failure so you know what not to do – or rather, what to proactively prevent (choose a good clinic, stick to aftercare, etc.) (gracetouchclinic.com).
My personal journey and deep dive into the research ultimately taught me that a hair transplant is equal parts science and art. The science gives us techniques to achieve high graft survival, and the art is in designing a result that looks naturally full and flattering. If you’re considering a hair transplant in Turkey or anywhere, arm yourself with knowledge. Insist on quality and don’t be shy about asking tough questions. A reputable clinic will welcome an informed patient. When you do it right, you’ll join those of us who look in the mirror every morning, smile at our new hair, and say “That was one of the best decisions I ever made.”
Sources: High-quality peer-reviewed studies, International Society of Hair Restoration Surgery (ISHRS) guidelines and warnings, Mayo Clinic Q&Anewsnetwork.mayoclinic.org, European Academy of Dermatology resources, and the author’s personal experience. (All factual claims backed by the cited references above.)

 Continue with Google
Continue with Google